【一般资料】
患者,女,25岁,
【主诉】
因头晕伴恶心呕吐10d,头痛5d加重2d入院。
【体格检查】
眼底检查视乳头水肿,双侧瞳孔等大等圆,对光反射灵敏。四肢肌力五级,肌张力不高,腱反射(+),病理征(-),颈软,脑膜刺激征(-)。
【辅助检查】
头颅MRI平扫示右侧颞叶、丘脑混杂T1、混杂T2信号,病灶边缘尚清,信号不均匀,增强后(图1~3)病灶呈斑片状强化。术后病理(图8A)提示:瘤细胞弥散分布,部分区域排列密集;瘤细胞胞浆淡染或透明,胞核居中;瘤细胞核呈圆形、卵圆形,核染色质深,有核异型性,核分裂象易见;瘤组织小血管丰富,管壁增生明显,呈大小不等的血管团;瘤组织中见大片坏死区域。免疫组化:瘤细胞Vim、Syn:+;Ki67:10%;CD34、SMA:血管壁+;EGFR:+;GST-π、T0P-Ⅱ:+;S100、Olig-2、GFAP、NF、Neu-N、EMA、IDH1:-;MGMT:-;P53:-。(右丘脑)结合临床及免疫组化结果,考虑为:(1)原始神经外胚层肿瘤(PNET,WHOⅣ级);(2)伴有间变特征的中枢神经细胞瘤(WHOⅢ级)。右丘脑肿瘤术后,患者行放疗化疗,定期复查头颅MRI,未见颅内肿瘤复发。一年后患者感双下肢乏力麻木,左下肢已不能自主活动,偶伴双下肢抽搐。专科查体:双上肢肌力Ⅴ°,左下肢肌力Ⅱ°,右下肢肌力Ⅴ-°,双上肢腱反射正常,右下肢膝反射及跟腱反射存在,左下肢膝反射消失,跟腱反射存在。双侧巴氏征(+),查氏征(+),双侧Hoffmann征(-)。背部T7~L2棘突及两侧皮肤触痛明显,双侧肋弓以下平面浅感觉减退,深感觉未及明显异常,颈软,无抵抗,脑膜刺激征(-),轮替试验稳准。胸腰椎MRI(图4~5)平扫示T8椎体平面髓外硬膜下见椭圆形等T1、稍长T2信号,脊髓受压,临近蛛网膜下腔增宽,增强后(图6~7)见T8、L2-3、L5平面椎管内病灶明显均匀强化,S1-2平面见类圆形囊性低信号。术前诊断:T8、L2-3及L5椎管内占位,结合既往影像符合神经纤维瘤病;骶管囊肿。术后病理(图8B)提示:瘤细胞弥散分布,排列密集;瘤细胞胞浆丰富淡染,部分胞浆透明,胞核呈圆形、卵圆形,核染色质深,核异型性明显,核分裂象可见;瘤组织血管丰富,部分管壁轻度增生;瘤组织中未见坏死区域。免疫组化:瘤细胞Vim、Syn:+;Ki67:25%;S100:少量细胞+;CD34、SMA、CD31:血管壁+;EGFR:+;GST-π、T0P-Ⅱ:+;Olig-2、GFAP、NF、Neu-N、EMA、CK、IDH1、CgA、Nestin:-;MGMT:-;P53:-。结合临床及免疫组化结果,考虑为:1.T8椎管内硬膜下,2.L2-3髓外,恶性肿瘤;考虑为:原始神经外胚层肿瘤(PNET,WHOⅣ级)。
【讨论】
患者MRI提示为幕上及椎管内病变。幕上原始神经外胚层肿瘤是一类非常罕见的发生于中枢神经系统的胚胎性肿瘤,大约仅占颅脑肿瘤的0.1%。文献报道幕上PNET典型者多发生于儿童,而在成人则发病率较低,本例发生于成人,较为少见。典型幕上PNET的MRI平扫常表现为体积较大的不均匀等、稍长T1及等、稍长T2信号肿块,囊变、坏死、出血、钙化、流空小血管影常见;肿瘤边界较清,瘤周水肿轻或无,增强扫描肿瘤实质呈明显均匀或不均匀强化。本例常需要与恶性脑膜瘤及胶质瘤进行鉴别诊断。由于PNET有高度侵袭性,软脑膜侵犯概率高。部分幕上PNET增强出现脑膜尾征,此时与脑膜瘤的鉴别比较困难。高级别的星形细胞瘤平扫常表现为不均匀长T1、长T2信号,囊变、坏死、出血多见,边界不清,水肿明显,呈不规则花瓣状明显强化,但强化程度低于PNET。本病例只进行了常规扫描,对肿瘤的定性有一定的偏差。若综合DWI(diffusion-weightedimaging)、MRS(magneticresonancespectrum)等MRI成像技术得到更全面的肿瘤相关信息,可以提高诊断准确率。有文献报道,PNETs在DWI上呈明显高信号,这可能与PNETs的细胞核浆比率高有关。PNETs的MRS显示胆碱含量升高,N-乙酰天门冬氨酸、丙氨酸、肌酸含量下降,可见脂质峰和肌醇峰,牛磺酸峰为其特征性峰。椎管内原始神经外胚层肿瘤以成人多见,硬膜内外均可发生,临床上多表现为脊髓压迫症状。MRI平扫多为均匀等T1、等T2信号,常呈长条状、分叶状或棒状,边界较清,中等程度强化,位于椎旁软组织内的肿瘤则边界不清。本例椎管内PNET需要和神经鞘瘤、转移瘤相鉴别。神经鞘瘤多位于硬膜下,呈长圆形,少数跨硬脊膜内外,形成特征性哑铃型外观,增强扫描强化显著,强化程度高于PNET。转移瘤好发于中老年人,肿块形态不规则,增强后多有环形强化,可伴邻近附件及椎体骨质破坏,结合原发肿瘤病史可鉴别。cPNET和pPNET均可发生在椎管内,两者的治疗方案和预后并发症有所不同,因此鉴别诊断非常重要。CD99作为PNET的标记物具有相对的特异性,对于鉴别中枢型和外周型PNET有一定意义。pPNET免疫组化染色CD99及神经内分泌标志物阳性,有些分化差者没有任何免疫组化标记,需通过电镜观察其分化特点。cPNET多由颅内原发灶沿脑脊液播散而来,CD99染色阴性,还需要结合细胞遗传学的方法进行确诊。那么,本例椎管内肿瘤是原发的,还是沿着脑脊液播散的?初次检查由于该患者无明显的下肢症状,手术前后都未意识到行全脊柱检查,无法确定当时椎管内有无肿瘤。但是结合颅内原发病史以及原始神经外胚层肿瘤高度恶性的特征,本例椎管内PNET高度怀疑是由原发于颅内的PNET经脑脊液播散转移所致。椎管内PNET可以是原发,但是比较罕见。也有部分椎管内PNET可以由颅内原发病灶沿脑脊液转移而来,临床工作中明确颅内PNET后建议进行全脊柱检查并按时复查随访,以尽早发现转移灶并及时治疗。文献报道,cPNET一旦发生脑脊液播散,预后比pPNET更差,平均生存期为1.5年,正规治疗后的5年生存率为46.9%。原发椎管内PNET也可能上行转移至颅内。因此,在明确诊断原发椎管内PNET之前应常规行头颅MRI检查以排除颅内PNET。原始神经外胚层肿瘤的临床症状和影像学表现缺乏特异性,确诊主要依靠病理检查联合免疫组织化学检查等。PNET光镜下为低分化的小圆形、卵圆形细胞,密集或成片排列,胞核为圆形或卵圆形,深染,核分裂像多见,胞浆少,部分肿瘤以Homer-Wright假菊形团结构及分叶状生长为其特征,部分可见明显的囊变、坏死。免疫组化显示神经细胞分化标志物阳性。CD99、神经元特异性烯醇化酶、FLI-1为诊断PNET的相对特异性的标志物。Ki67代表肿瘤细胞的增殖活性。文献报道Ki67大于30%的PNET患者术后平均生存期为8个月。PNET恶性程度高,极易复发转移,因此早期发现、准确诊断和联合治疗非常重要。手术联合放化疗可作为原始神经外胚层肿瘤患者标准的治疗方法,术后高强度化疗是减少远处转移的最佳方案。
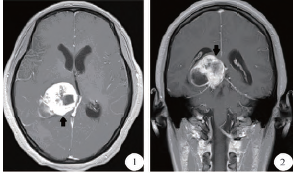

图1~3 MRI增强扫描可见轴位、冠状位、矢状位,右侧颞叶、丘脑处类圆形病灶,呈斑片状不均匀强化,边界清楚,中线结构左移

图8A:瘤组织小血管丰富,管壁增生明显,呈大小不等的血管团,瘤组织中见大片坏死区域;

图4、图5平扫示T8椎体平面髓外硬膜下见椭圆形等T1、稍长T2信号,边界清,脊髓受压,临近蛛网膜下腔增宽;图6增强后见T8平面椎管内病灶明显均匀强化;图7腰椎增强后见L2-3、L5平面椎管内病灶明显均匀强化,边界尚清,S1-2平面见类圆形未强化的囊性低信号

图8B:瘤组织血管丰富,部分管壁轻度增生;瘤组织中未见坏死区域
原始出处:
戴珂,肖朝勇,胡新华.幕上及椎管内原始神经外胚层肿瘤1例并文献复习[J].临床神经外科杂志,2017,14(4):247-250.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#椎管内#
31
#椎管#
25
学习了.谢谢作者分享!
0
学习了.谢谢作者分享!
104
不错的病理.谢谢
95
努力学习.天天向上
96