J Dermatolog Treat:利用第3期临床试验中患者水平的银屑病面积和严重程度指数评分来分析疾病活动和治疗效果
2022-04-08 MedSci原创 MedSci原创
最近,有几种新药被批准用于治疗中度至重度斑块状银屑病。随着选择的增加,为每个病人选择最合适的治疗方法的挑战也在增加。
最近,有几种新药被批准用于治疗中度至重度斑块状银屑病。随着选择的增加,为每个病人选择最合适的治疗方法的挑战也在增加。治疗的疗效可从2个广泛的角度来看:与基线相比,银屑病严重程度的相对改善,以及治疗期间的残留疾病活动。目前尚不清楚斑块状银屑病临床试验的主要疗效结果是否代表治疗期间的残留疾病。近日,发表于J Dermatolog Treat的研究评估了用残余疾病活动来补充二分法疗效。
这项事后分析使用了来自reSURFACE 1/2 (NCT01722331/NCT01729754)3期临床试验的中度至重度斑块状银屑病患者的替拉珠单抗 100 mg(N = 616)或安慰剂(N = 309)治疗后的汇总患者的水平数据。
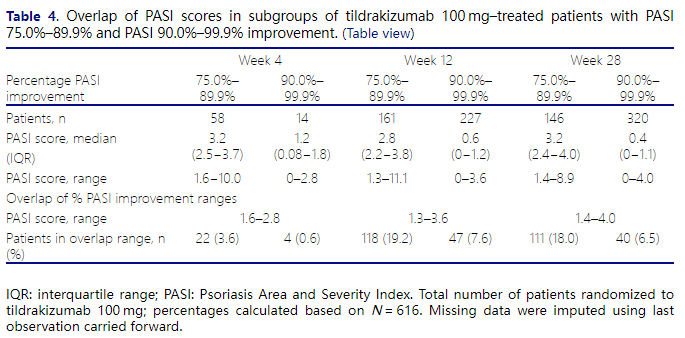
结果,接受替拉珠单抗 100毫克的患者基线银屑病面积和严重程度指数(PASI)中位数为17.9。在第12周,中位PASI为2.9,而二分法PASI 90反应率为36.9%,绝对PASI<5.0、<3.0和<1.0的比例分别为64.0%、50.8%和23.3%。在第28周,中位PASI为1.7,而PASI 90反应率为51.9%,绝对PASI<5.0、<3.0和<1.0的比例分别为75.3%、62.8%和38.0%。在第28周之前,皮肤病生活质量指数和PASI评分是相关的(r=0.51,p≤0.0001)。
综上所述,该研究结果表明,通过PASI评分估计疾病活动性比PASI改善百分比更可靠;这或许是导致临床试验和实践之间疗效差异的部分原因。这些结果表明,使用PASI评分补充二分法的PASI改善,并考虑患者的治疗目标,可以促进临床决策的制定。
原始出处:
K B Gordon, et al., Disease activity and treatment efficacy using patient-level Psoriasis Area and Severity Index scores from tildrakizumab phase 3 clinical trials. J Dermatolog Treat. 2022 Feb;33(1):219-228. doi: 10.1080/09546634.2020.1747590.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#3期临床#
52
#TREAT#
53
#疾病活动#
40
#治疗效果#
36
#3期临床试验#
49