盘点:近期非酒精性脂肪肝治疗新近进展
2016-08-18 MedSci MedSci原创
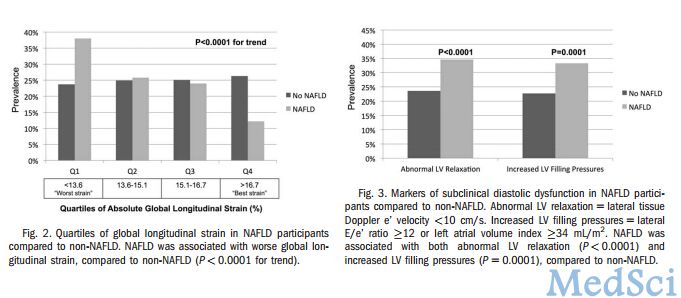
脂肪肝,是指由于各种原因引起的肝细胞内脂肪堆积过多的病变。脂肪性肝病正严重威胁国人的健康,成为仅次于病毒性肝炎的第二大肝病。脂肪肝是一种常见的临床现象,而非一种独立的疾病。其临床表现轻者无症状,重者病情凶猛。非酒精性脂肪性肝病(NAFLD)是指除外酒精和其他明确的损肝因素所致的肝细胞内脂肪过度沉积为主要特征的临床病理综合征,与胰岛素抵抗和遗传易感性密切相关的获得性代谢应激性肝损伤。非酒精性脂肪


本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#酒精性脂肪肝#
32
#酒精性#
38
#非酒精性#
43
文章不错,继续学习
80
学习学习。。。
79
很好,不错,以后会多学习
66
谢谢分享,学习了
80
这篇资讯带给我们新知识,启发新思维,不论是科研还是临床工作都有很大的帮助。。。
77
这篇资讯写的真好,带给我们新知识,启发新思维,不论是科研还是临床工作都有很大的帮助。。。
34
这篇资讯写的真好,带给我们新知识,启发新思维,不论是科研还是临床工作都有很大的帮助。。。
39