(12号)Radiology:在CTA中使用深度学习进行主动脉夹层的识别及Stanford分类
2022-02-09 shaosai MedSci原创
临床上,主动脉夹层(AD)是急性主动脉综合征最常见的原因之一,约总数的85%至95%。AD的年发病率约为每10万人中2.9至4.3人。
 临床上,主动脉夹层(AD)是急性主动脉综合征最常见的原因之一,约总数的85%至95%。AD的年发病率约为每10万人中2.9至4.3人。Stanford 分类法是最常用的分类方法之一,A型AD累及升主动脉,有或没有累及降主动脉,B型AD累及左锁骨下动脉远端的降胸主动脉。如果不接受治疗,A型AD在症状出现后每小时的死亡率为1-2%,48小时内超过50%;因此,AD的早期和准确的诊断是挽救生命的关键。现阶段,主动脉的计算机断层扫描(CTA)已成为评估AD的一线方式。
临床上,主动脉夹层(AD)是急性主动脉综合征最常见的原因之一,约总数的85%至95%。AD的年发病率约为每10万人中2.9至4.3人。Stanford 分类法是最常用的分类方法之一,A型AD累及升主动脉,有或没有累及降主动脉,B型AD累及左锁骨下动脉远端的降胸主动脉。如果不接受治疗,A型AD在症状出现后每小时的死亡率为1-2%,48小时内超过50%;因此,AD的早期和准确的诊断是挽救生命的关键。现阶段,主动脉的计算机断层扫描(CTA)已成为评估AD的一线方式。
现阶段,深度学习卷积神经网络(CNN)在医学图像分析中表现出良好的诊断性能。深度学习通过在像素水平上表达和提取原始数据的特征来建立复杂的模型构建,并捕捉到图像和诊断之间的复杂关系。目前的AD研究在分割和检测方面受到限制。
近日,发表在Radiology杂志的一项研提出了一个2步分层模型,评估了深度学习神经网络对AD检测和分类的诊断性能,为临床AD的早期、快速筛查提供了技术支持。
本研究于2015年至2019年期间,收集了主动脉CTA中的130个动脉相位系列(57个A型,43个B型,30个阴性病例)用于训练和验证。建立了一个2个步骤的分层模型,包括第一步检测AD,第二步预测Stanford分型(0-1)。该模型的性能在2020年通过一个离线的前瞻性测试进行评估。报告了Stanford A型、B型和无AD(分别为Sens A, B, N和Spec A, B, N)的敏感性和特异性以及Cohen's kappa。
在离线前瞻性测试的298例(22例A型,29例B型,247例无AD)中,Sens A、Sens B和Sens N分别为95.45%(95%置信区间[CI],77.16-99.88%),79.31%(95%CI,60.28-92.01%)和93.52%(95%CI,89.69-96.25%)。Sens A、Sens B和Sens N分别为98.55%(95%CI,96.33-99.60%)、94.05%(95%CI,90.52-96.56%)和94.12%(95%CI,83.76-98.77%)。分型率达到92.28%(95%CI,88.64-95.04%)。Cohen's kappa为0.766(95% CI, 0.68-0.85; p < 0.001)。
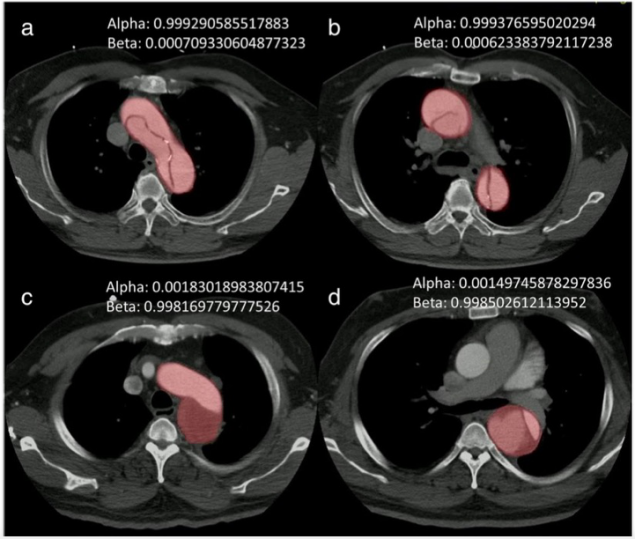
图 Stanford A型和B型主动脉夹层(AD)的示例。在主动脉CTA的动脉相轴位图像上,Stanford A型AD显示撕裂口累及主动脉弓(a)和升、降胸主动脉(b)。Stanford B型AD显示撕裂口在主动脉弓(c)和降胸主动脉(d)处延伸到左锁骨下动脉,而不累及升胸主动脉。输出 "Alpha "和 "Beta "的概率(0-1)并显示在右上角,分别代表升主动脉和降主动脉的受累情况。
本项研究表明,深度学习CNN可以在主动脉CTA图像上对AD进行并进行准确的Stanford分型,可实现在紧急情况下协助临床医生对病人自动风险分层的潜力。
原文出处:
Li-Ting Huang,Yi-Shan Tsai,Cheng-Fu Liou,et al.Automated Stanford classification of aortic dissection using a 2-step hierarchical neural network at computed tomography angiography.DOI:10.1007/s00330-021-08370-2
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Stanford#
42
#CTA#
40
#主动脉#
41
#动脉夹层#
36