Heart:无阻塞性冠状动脉心肌梗死患者结局分析
2018-09-30 xing.T MedSci原创
由此可见,MINOCA较为常见,其不良结局率约为阻塞性CAD患者的一半。死亡的主要原因是非CVD死亡。MINOCA患者的事件发生率明显高于没有CVD的人群。
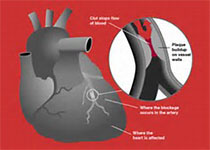
非梗阻性冠状动脉(MINOCA)心肌梗死患者的中期结果和死因尚未得到很好的总结归纳。近日,心脏病领域权威杂志Heart上发表了一篇研究文章,该研究的目的是比较梗死性冠状动脉疾病(CAD)心肌梗死患者和MINOCA患者的死亡率和复发事件发生率,并与未患心血管疾病(CVD)的年龄和性别匹配队列进行比较。
研究人员对2013年至2015年期间全新西兰急性冠状动脉综合征-质量改进(ANZACS QI)登记处2年内接受冠状动脉造影的患者进行了一项全国队列研究。MI患者登记数据与国家住院和死亡率记录相关联。没有已知CVD的年龄和性别匹配的患者组成对照组。
在8305名MI患者中,897名(10.8%)患者被归类为MINOCA。与没有已知CVD的患者相比,阻塞性CAD患者的主要结局(全因死亡或复发性非致命性MI)的调整后HR为7.81(95%CI为6.64-9.19,p<0.0001),MINOCA患者为4.64(95%CI为3.54-6.10,p<0.0001)。阻塞性CAD患者2年时Kaplan-Meier全因死亡率为7.9%,其中近一半为CVD死亡患者(分别为3.6%CVD死亡和4.5%非CVD死亡)。相比之下,MINOCA患者全因死亡率为4.9%,以非CVD死亡(4.5%)为主。
由此可见,MINOCA较为常见,其不良结局率约为阻塞性CAD患者的一半。死亡的主要原因是非CVD死亡。MINOCA患者的事件发生率明显高于没有CVD的人群。
原始出处:
Michael J A Williams.et al. Outcome after myocardial infarction without obstructive coronary artery disease.Heart. 2018. http://dx.doi.org/10.1136/heartjnl-2018-313665
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#阻塞#
34
#ART#
21
#患者结局#
23
#HEART#
25