BMC Cancer:双药对比三药新辅助治疗局部进展期胃癌(LAGC)的疗效:倾向评分匹配(PSM)研究
2021-12-15 yd2015 MedSci原创
研究表明,与双药方案相比,三药新辅助治疗方案并没有带来额外的生存获益。它甚至可能导致更高的术后并发症的风险。
胃癌是全球第五大最常见的恶性肿瘤,也是癌症相关死亡的第三大原因。大多数患者诊断时为晚期,预后极差。对于可手术的局部进展期胃癌(LAGC),建议采用新辅助化疗(NAC)。然而,在不同的指南中,推荐的治疗方案差别很大。近期,来自中山大学附属第六医院的团队开展了相关回顾性研究,评估三药对比双药新辅助(NAC)治疗局部进展期胃癌(LAGC)患者的疗效。相关结果发表在BMC Cancer杂志上。
本文回顾了227例接受NAC及后续胃癌根治术的局部进展期胃癌(LAGC)患者。通过倾向评分匹配(PSM),选择140例基线特征相似的患者。其中70例采用含铂+氟尿嘧啶双药方案;另外70人接受多西他赛、铂和氟尿嘧啶三药方案。
FLOT和SOX是研究常用方案,占90%。其他方案包括FOLFOX、CAPOX、DCF方案,均为临床常用方案。所有患者术前平均接受4个周期的NAC治疗。PSM前后,三药治疗队列中性粒细胞减少和贫血发生率较高,而血小板减少在双药队列中更为常见。3/4级血液学毒性的发生率差异无统计学意义。
两组R0切除率无明显差异(双药组90.1%,82/91;三药组88.2%,120/136,p = 0.829)。PSM匹配后,双药组和三药组的R0切除率相似(均为88.6%,62/70,p = 0.1)。三药组的并发症发生率(Clavien-Dindo 2 - 4级)显著高于对照组(PSM前:双药8.8%,8/91 vs三药27.2%,37/136,p = 0.001;PSM后:双药5.7%,4/70 vs三药27.1%,19/70,p = 0.001),尤其是外科相关的腹部感染,主要由吻合口瘘引起。至于病理结果,两个队列的TRG在PSM分析之前和之后在统计学上是相似的。三药治疗的病理完全缓解率较高(0级:PSM前,双药 11.0%, 10/91; 三药 16.2%, 22/136, p = 0.686; PSM后,双药11.4%, 8/70;三药 15.7%,11/70, p = 0.642),但差异没有统计学差异。

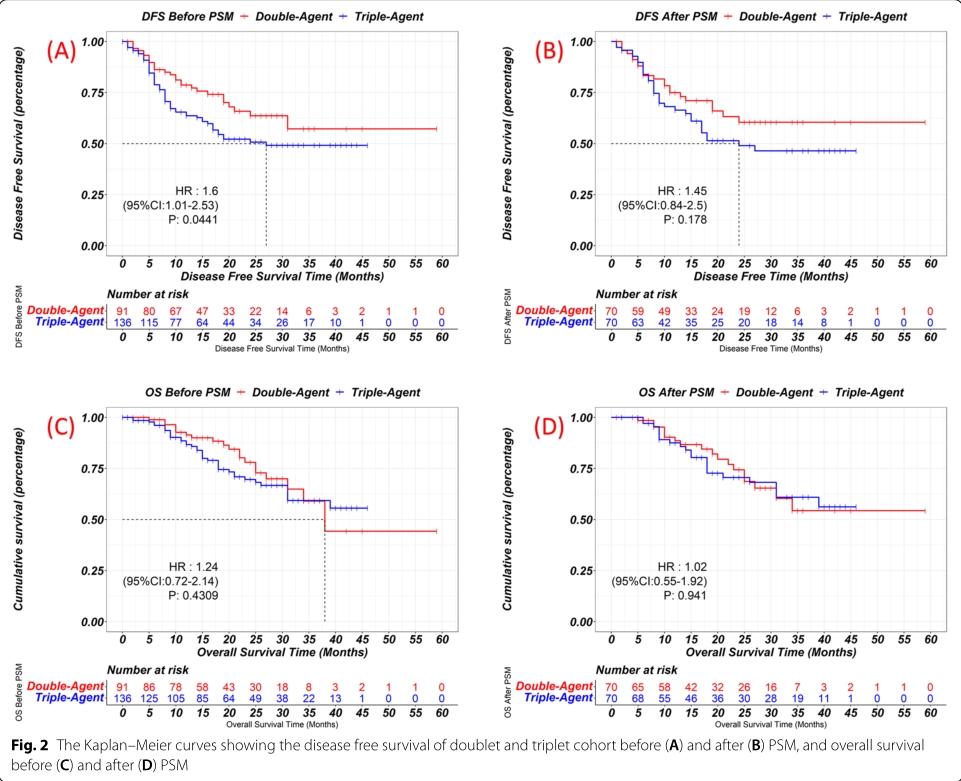
中位随访时间为31个月。PSM前三药组的无病生存期(DFS)较短,但PSM后差异不显著(1年DFS率,双药 77.1% vs. 三药 68.6%, p = 0.178)。两组患者在PSM前后的总生存期(OS)相似(PSM后3年OS率,双药54.3% vs三药60.9%, p = 0.941)。
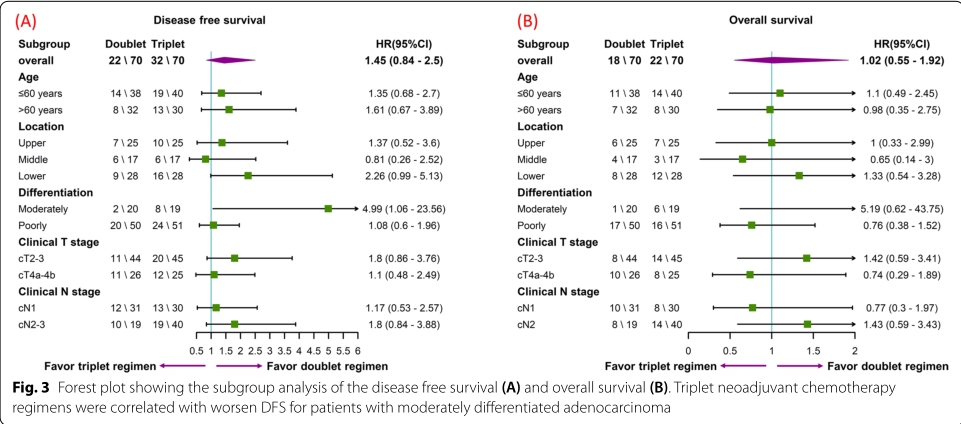
在亚组生存分析中,三药治疗队列在任何亚组中也没有表现出任何优势。在中分化腺癌亚组患者中,三药NAC甚至与DFS缩短相关。因此,这些数据表明,与双药方案相比,三药方案并没有带来额外的生存效益。
综上,研究表明,与双药方案相比,三药新辅助治疗方案并没有带来额外的生存获益。它甚至可能导致更高的术后并发症的风险。
原始出处:
Yonghe Chen , Jiasheng He, Dan Liu, et al. Triplet versus doublet neoadjuvant chemotherapy regimens for locally advanced gastric cancer: a propensity score matching analysis. BMC Cancer (2021) 21:1328 https://doi.org/10.1186/s12885-021-09093-9
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#新辅助#
28
#进展期#
38
#BMC#
30
#倾向评分匹配#
26
学习了,谢谢分享
47
于广泛期SCLC患者,铂类为基础的化疗是
58
#局部#
26