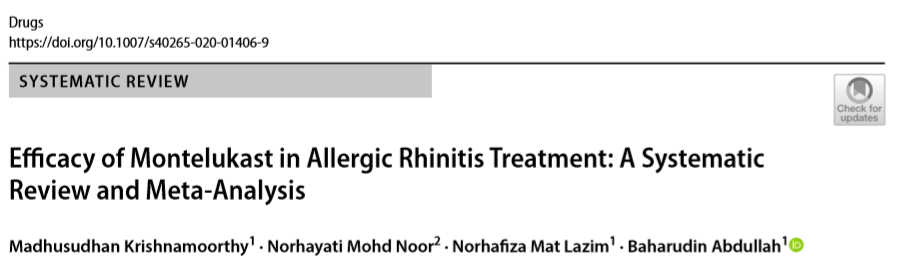
Drugs:孟鲁司特治疗变应性鼻炎的疗效:系统综述和荟萃分析
2020-09-28 AlexYang MedSci原创
在治疗变应性鼻炎时,孟鲁司特有可能作为口服抗组胺剂或鼻内皮质类固醇的替代品或添加剂使用。本系统综述评估了孟鲁司特治疗变应性鼻炎的有效性。
在治疗变应性鼻炎时,孟鲁司特有可能作为口服抗组胺剂或鼻内皮质类固醇的替代品或添加剂使用。本系统综述评估了孟鲁司特治疗变应性鼻炎的有效性。
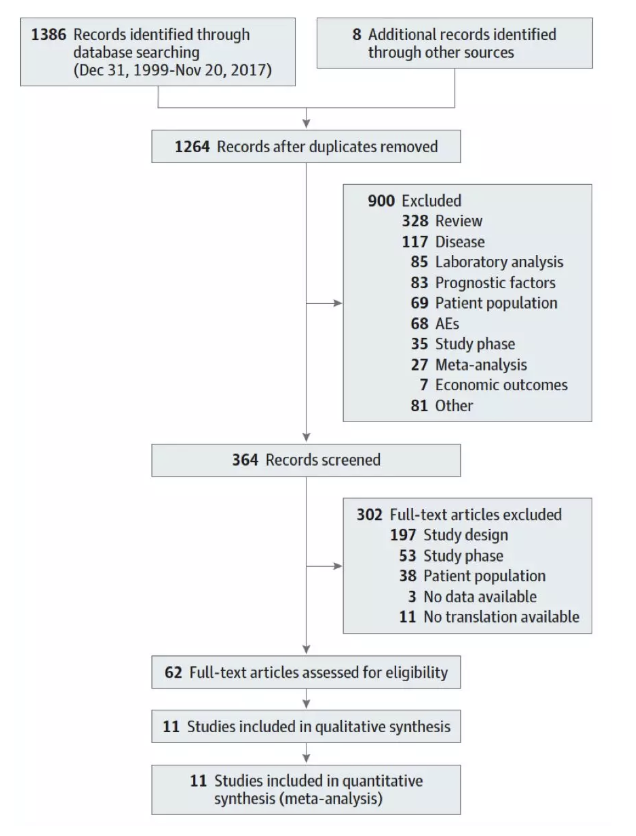
研究人员使用Cochrane中心从1966年到2019年1月21日登记的对照试验、EMBASE和MEDLINE进行电子文献检索。入选标准是比较孟鲁司特与安慰剂或其他标准治疗的随机对照试验。主要评估结果为日间鼻部症状评分(DNS)和夜间鼻部症状评分(NNS)。次要评估结果为综合鼻症状评分(CSS)、日间眼睛症状评分(DES)和鼻结膜炎生活质量问卷(RQLQ)。他们采用基于随机效应模型的Review Manager 5.3软件进行meta分析。
15项研究的10387名参与者符合纳入标准。结果显示,孟鲁司特改善DNS(平均差异[MD] - 0.12, 95%置信区间[CI] - 0.15 ~ - 0.08;p < 0.001)、NNS (MD - 0.09, 95% CI - 0.13 ~ - 0.05;p < 0.001)、CSS (MD - 0.08, 95% CI - 0.11 ~ - 0.06;p < 0.001)、DES (MD - 0.17, 95% CI - 0.33 ~ - 0.02;p < 0.030)和RQLQ (MD - 0.34, 95% CI - 0.49 ~ - 0.20;p < 0.001)的效果均优于安慰剂。口服抗组胺剂(OAH)改善DNS(MD 0.08, 95% CI 0.03-0.13;p = 0.002)、 CSS (MD 0.03, 95% CI - 0.02 ~ 0.07;p = 0.27)、DES (MD 0.06, 95% CI 0-0.12;p = 0.040),和RQLQ (MD 0.03, 95% CI - 0.05 ~ 0.12;p = 0.430)的效果优于孟鲁司特。孟鲁司特对NNS(MD -0.03, 95% CI - 0.08 ~ 0.03;p = 0.330)的改善优于口服抗组胺剂。氟替卡松鼻喷剂对DNS(MD 0.71, 95% CI 0.44-0.99;p < 0.001)和NNS (MD 0.63, 95% CI 0.29-0.97;p < 0.001)的改善效果优于孟鲁司特。孟鲁司特联合口服抗组胺剂改善DNS(MD - 0.15, 95% CI - 0.27 ~ - 0.03; p = 0.010)、NNS (MD - 0.16, 95% CI - 0.28 ~ - 0.05;p = 0.006)、CSS (MD - 0.12, 95% CI - 0.25~- 0.01;p = 0.070、DES (MD - 0.12, 95% CI - 0.30 - 0.06;;p = 0.180)和RQLQ (MD - 0.10, 95% CI - 0.28 - 0.08;p = 0.290)的效果优于口服抗组胺剂。孟鲁司特联合OAH改善DNS(MD 0.15, 95% CI 0.08-0.21; p < 0.001)、NNS (MD 0.05, 95% CI - 0.09 ~ 0.19;p = 0.510)、CSS (MD 0.1, 95% CI 0.03-0.17;p = 0.007)、 DES (MD 0.18, 95% CI 0-0.36;p = 0.050)和RQLQ (MD 0.07 95% CI - 0.15 ~ 0.29;p = 0.530)的效果优于孟鲁司特。
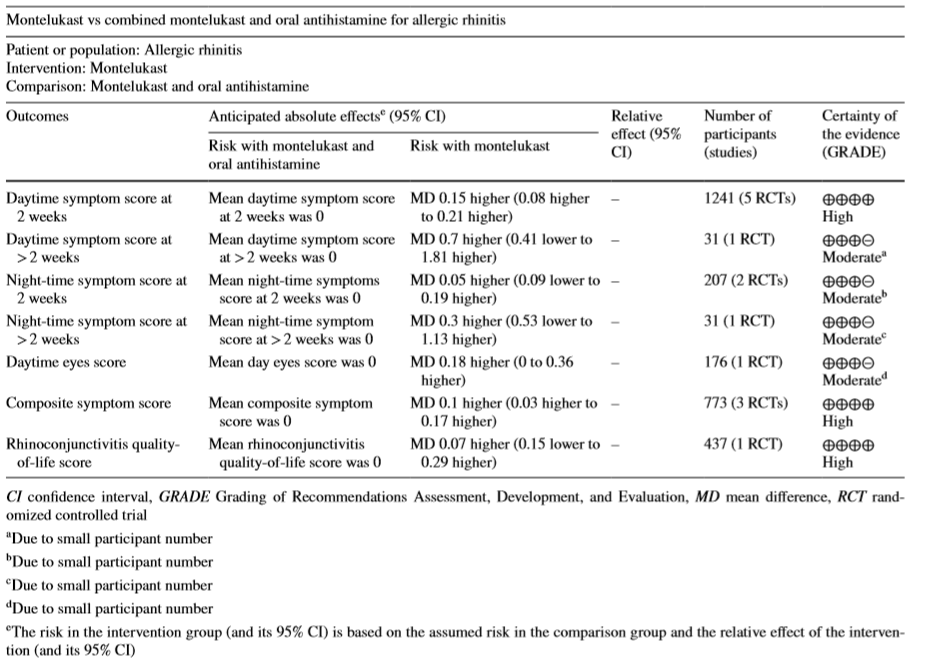
孟鲁司特与孟鲁司特联用口服抗组胺药发现总结
该研究表明,对于变应性鼻炎的整体症状,孟鲁司特比安慰剂更有效,而孟鲁司特与口服抗组胺药联合治疗优于单独口服抗组胺药或孟鲁司特联合治疗。
原始出处:
Krishnamoorthy M, Mohd Noor N, Mat Lazim N, Abdullah B. Efficacy of Montelukast in Allergic Rhinitis Treatment: A Systematic Review and Meta-Analysis. Drugs. 2020 Sep 11
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Drug#
37
#drugs#
38
#系统综述#
42
#荟萃#
31
#荟萃分析#
39
#孟鲁司特#
31
#变应性鼻炎#
29
谢谢梅斯提供这么好的信息,学到很多
0