Macromol Biosci:无细胞各向异性支架原位诱导软骨-软骨下骨缺损再生
2017-05-28 佚名 MaterialsViews
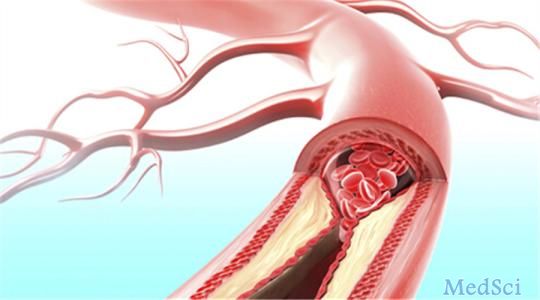
骨软骨缺损会导致软骨层及软骨下骨的破坏。由于特殊的物理结构,生物体难以自发实现骨软骨缺损结构和功能的再生。生物材料支架可为组织再生提供时间及空间维度上的支撑。具有取向孔的支架能够促进细胞在支架中的迁移和有序排列,提高新生组织与原有组织间的信号沟通,诱导新生组织结构的形成和功能重塑。浙江大学高长有教授及其合作者采用定向冷冻结晶的方法制备了具有径向取向孔的甲基丙烯酸化透明质酸支架,通过光交联稳定了支架
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#CRO#
22
#MAC#
26
#Bio#
35
#ACR#
27
#骨缺损#
34
学习了,谢谢分享!
41
学习了谢谢分享。
60
谢谢分享谢谢分享
52