EHP:证实无机砷诱导的癌细胞可将正常干细胞转化为癌干细胞
2012-04-10 towersimper 生物谷
科学家早已证实无机砷是一种人类致癌剂。另外,越来越多的证据提示着癌症是一种基于干细胞的疾病。正常的干细胞是组织再生和有机体维持稳定性所必需的。但是癌干细胞被认为是肿瘤形成、生长和扩散的驱动力。 来自美国国家环境卫生科学研究所分支机构国家环境卫生科学研究所(National Institute of Environmental Health Sciences)国家毒理检测实验室(National
科学家早已证实无机砷是一种人类致癌剂。另外,越来越多的证据提示着癌症是一种基于干细胞的疾病。正常的干细胞是组织再生和有机体维持稳定性所必需的。但是癌干细胞被认为是肿瘤形成、生长和扩散的驱动力。
来自美国国家环境卫生科学研究所分支机构国家环境卫生科学研究所(National Institute of Environmental Health Sciences)国家毒理检测实验室(National Toxicology Program Laboratory)的Michael Waalkes博士和他的研究小组之前已经发现正常细胞当用无机砷处理后就变成癌细胞。在这项新研究中,研究人员发现当把这些癌细胞放在正常的干细胞附近而且不相互接触时,这些正常的干细胞非常快地获得癌干细胞的特征。这就证实癌细胞能够通过半通透性细胞膜发送分子信号,从而将正常的干细胞变成癌干细胞。

这篇论文证实癌症能够通过招募附近的正常干细胞并过量产生癌干细胞来进行增殖。招募正常的干细胞并将之变成癌干细胞可能在包括癌症生长和转移在内的致癌过程中产生极其广泛的影响。这也意味着干细胞有助于解释致癌作用的产生机理,而且它们也可能是其他慢性疾病的影响因素。
这些发现揭示砷致癌的一个潜在重要性的机制,可能有助于解释一些研究砷的研究人员的观察结果:砷经常导致多种类型的肿瘤在皮肤上或身体内形成。
在这项研究中,研究人员使用前列腺干细胞系而不是胚胎干细胞来进行研究。相关研究结果于2012年4月4日在线发表在Environmental Health Perspectives期刊上。(生物谷:towersimper编译)

doi:10.1289/ehp.1204987
PMC:
PMID:
Arsenic-Transformed Malignant Prostate Epithelia Can Convert Noncontiguous Normal Stem Cells into an Oncogenic Phenotype
Yuanyuan Xu, Erik J. Tokar, Yang Sun, Michael P. Waalkes
Background: Cancer stem cells (CSCs) are likely critical to carcinogenesis, and, like normal stem cells (NSCs), are impacted by microenvironment. Malignant cells release extracellular factors modifying tumor behavior. Inorganic arsenic, a human carcinogen, over-produces CSCs in various model systems of carcinogenesis. Here, we determine if NSCs are influenced by nearby arsenic-transformed malignant epithelial cells (MECs) as a possible factor in arsenic associated CSC overabundance.
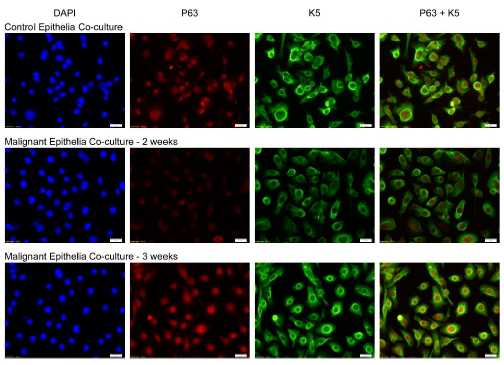
Methods: Transwell non-contact co-culture allowed the study of the effects of non-contiguous, arsenic-transformed prostate MECs on the isogenic human prostate NSC line, WPE-stem. Cancer phenotype was assessed by secreted MMPs, invasiveness, colony formation and spheroid formation. Gene expression was assessed at the protein (western blot) or mRNA (RT-PCR) levels.
Results: Non-contact co-culture of MECs and NSCs rapidly (≤ 3 weeks) caused hyper-secretion of MMPs and marked suppression of the tumor suppressor gene PTEN in NSCs. NSCs co-cultured with MECs also showed increased invasiveness and clonogenicity and formed more free-floating spheroids and highly branched ductal-like structures in Matrigel, all typical for CSCs. MEC co-culture caused dysregulated self-renewal and differentiation-related gene expression patterns and epithelial-to-mesenchymal transition in NSCs consistent with acquired cancer phenotype. Interleukin-6, a cytokine involved in tumor microenvironment control, was hyper-secreted by MECs and interleukin-6 exposure duplicated several responses in NSCs of conversion to CSCs via MEC co-culture (MMP hyper-secretion, decreased PTEN, etc.).
Conclusions: These results indicate that arsenic-transformed MECs recruit nearby NSCs into a cancer phenotype thereby potentially increasing CSC number. This may be a factor in arsenic-induced CSC overabundance seen in multiple model systems.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#EHP#
32
#癌细胞#
33
#癌干细胞#
40
#砷#
28