柳叶刀揭示西班牙疫苗混打AZ疫苗与辉瑞疫苗后特异性抗体显著增高
2021-06-28 JACKZHAO MedSci原创
柳叶刀于2021年6月25日在线发表了一篇研究,本研究旨在评估
https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(21)01420-3/fulltext
6月25日《柳叶刀》在线发表了旨在评估第一针接种ChAdOx1-S疫苗第二针接种BNT162b2疫苗人群的免疫原性和反应原性研究,该研究是首个评估异源疫苗接种免疫原性和反应原性的临床研究。
该研究(CombiVacS)主要在西班牙五所大学附属医院进行,是一项多中心、开放标签、随机对照的II期研究,该研究已在EudraCT(2021-001978-37)和 ClinicalTrials.gov(NCT04860739)注册,研究还在进行中。
研究招募对象为年龄在 18-60 岁、在筛查前 8-12 周接种单剂 ChAdOx1-S疫苗 且无 SARS-CoV-2 感染史的成年人。符合入选标准的人按照2:1被随机分配到干预组和对照组,干预组人群将接种接受一次BNT162b2(0.3 mL),对照组无干预措施。通过收集研究对象的接种疫苗当天、第7天、第14天的不良反应事件和血标本,进行免疫原性和反应原性方面的评估。通过比较接种BNT162b2疫苗后14 天针对新冠病毒RBD和S抗原特异性抗体的差异,次要结果是采用假病毒中和试验评估抗体功能,并使用干扰素-γ 免疫试验评估细胞免疫反应。反应原性结果是评估接种BNT162b2后7天内的局部和全身不良事件。
在2021年4月24日至30日期间,在西班牙的五所大学附属医院共招募了 676 名符合入选标准的研究对象,平均年龄为44岁,382名(57%)为 女性,294名(43%)为男性。研究对象按照2:1随机分配到干预组(n=450)或对照组(n=226)。最后663(98%)名参与者(干预组441名,对照组222名)在第 14 天完成了研究。
研究结果发现,异源疫苗接种第 14 天新冠病毒RBD特异性抗体滴度的几何平均值在两组之间有显著性差异:干预组RBD特异性抗体平均为7756.68 BAU/mL(95% CI 7371.53-8161.96),对照组平均为99.84 BAU/mL(95% CI :76.93-129.59);干预组是对照组的77.69倍(95% CI 59.57-101.32)。另外,接种第 14 天新冠病毒S抗原特异性抗体的滴度在两组之间也有显著性差异:干预组S抗原特异性抗体平均为3684.87 BAU/mL(95% CI 3429.87-3958.83),对照组平均为101.2BAU/mL(95% CI :82.45–124.22);干预组是对照组的 36.41倍(95% CI 29.31–45.23;p<0·0001)。

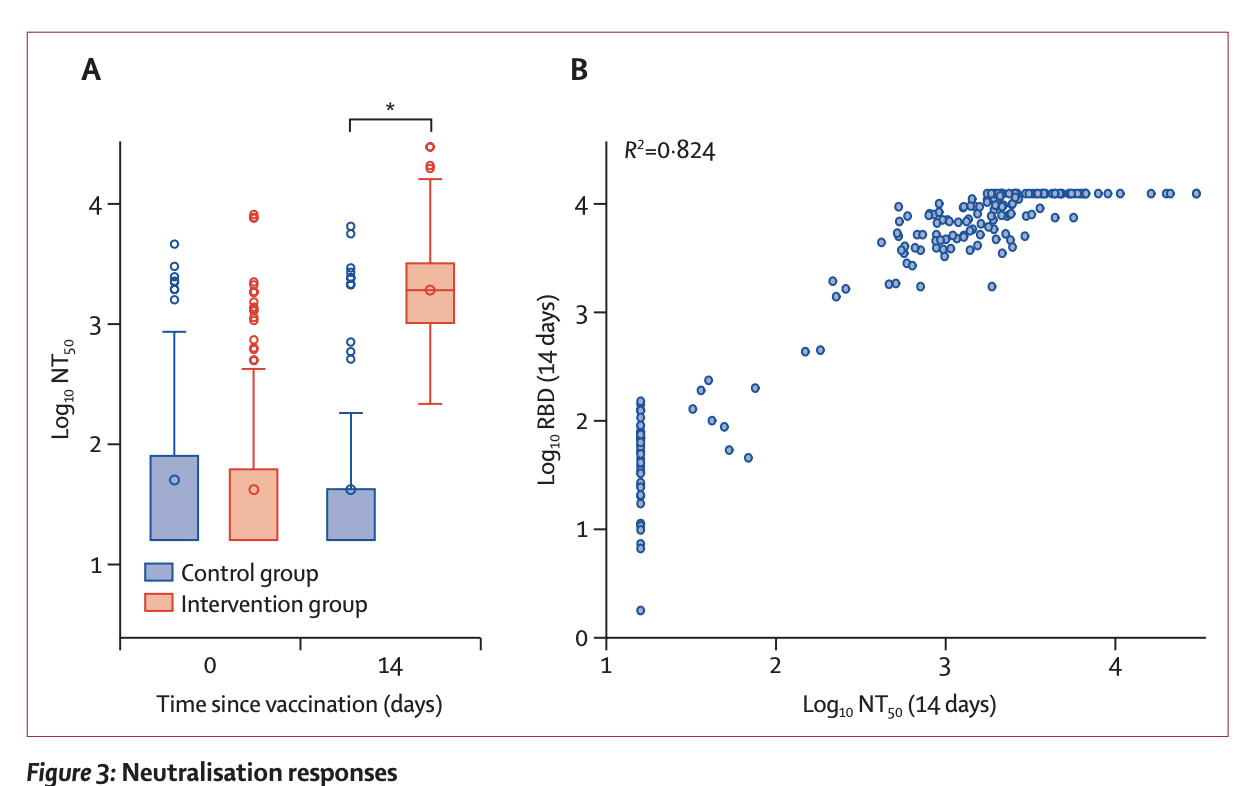
研究通过假病毒中和试验评估抗体功能的实验发现,干预组中和抗体的平均数较基线水平增加了 45 倍,而对照组中和抗体活性在第14天与基线相比无显著差异。
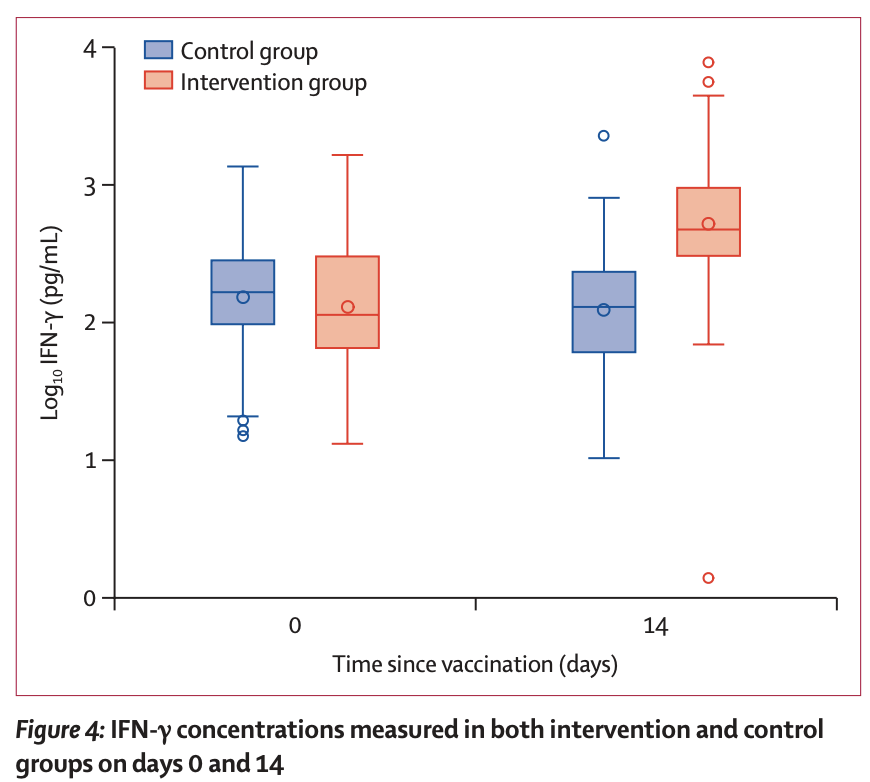
在细胞免疫方面,该研究在 151 名研究对象(n=99 干预组,n=52 对照组)中评估了功能性S抗原特异性 T 细胞反应的动态变化。研究发现,第 0 天干预组的 IFN-γ释放值平均为129.63 pg/mL(95% CI 103.51-162.35),对照组 IFN-γ平均为 151.63 pg/mL(95% CI 114.09-201.53)。在异源疫苗接种第 14 天,干预组的 IFN-γ 产生显著增加,平均为521.22 pg/mL(95% CI 422.44-643.09),而对照组IFN-γ 产生无明显变化,平均为122.67 pg/ml(95% CI 88.55-169.95)。
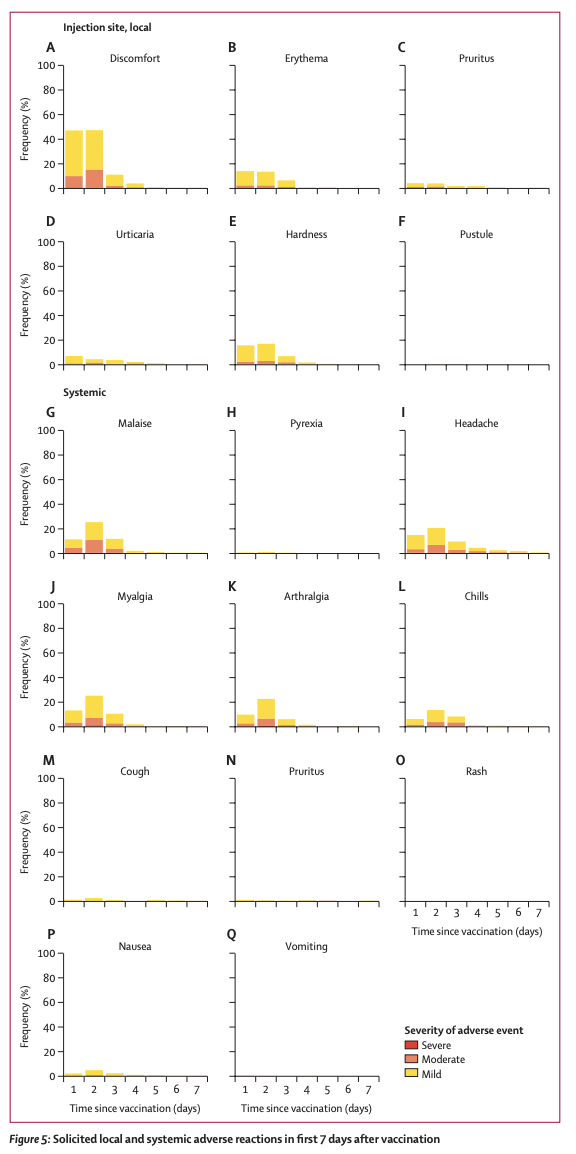
反应原性分析基于干预组 448 名个体中征集的不良事件分析。最常见的全身反应包括头痛(n=199 [44%])、肌痛(n=194 [43%])和不适(n=187 [42%]),其他相对少见的全身不良反应为发烧 (n=11 [2%])。局部不良反应最常见的包括注射部位疼痛(n=395 [88%])、硬结(n=159 [35%])和红斑(n=139 [31%])。在干预组接种疫苗后 7 天内报告的 1771 起不良事件中,大多数为轻度 (n=1210 [68%]) 或中度 (n=530 [30%]),并且是自限性的,没有严重的不良事件的报告。
该研究表明,在第一剂接种ChAdOx1-S疫苗的个体8-12周后予以第二剂接种BNT162b2疫苗后14 天的体液免疫和细胞免疫反应显著增加,异源疫苗接种能够极大程度增强疫苗接种效果,产生高滴度抗体。不过该研究只进行了单独接种ChAdOx1-S疫苗和混合接种ChAdOx1-S+BNT162b2这两组人群对比,并没有与接种两次BNT162b2疫苗或者接种两次ChAdOx1-S疫苗的人群进行免疫反应的对比。
文章指出,这是第一份报告显示COVID-19 异源疫苗接种计划诱导人体的免疫反应与可接受和可控的反应原性特征。 这在第二次给药后 7 天获得早期反应,并且在第 14 天确认,显示出与异种方案。 特别是,有一个强大的评估的免疫反应之间的一致性针对 SARS-CoV-2 尖峰的特异性抗体的滴度蛋白质和功能的比例增加相应测试中的中和能力。之间观察到很强的正相关两种免疫测定和假病毒中和测定。 免疫细胞反应 14 天后加强疫苗也为有效性提供支持的异源方法。
该研究还在进行中;未来比较同源和异源疫苗接种的研究结果会陆续公布,可能会对疫苗接种策略具有一定的参考意义。
参考文献:
Immunogenicity and reactogenicity of BNT162b2 booster in ChAdOx1-S-primed participants (CombiVacS): a multicentre, open-label, randomised, controlled, phase 2 trial. Lancet. Published Online June 25, 2021 DOI: https://doi.org/10.1016/ S0140-6736(21)01420-3
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#特异性#
31
#AZ#
32
#特异性抗体#
34
#增高#
0
#增高#
33