JASN:社区供水系统铅浓度与晚期CKD患者血红蛋白浓度之间的关联
2021-08-08 MedSci原创 MedSci原创
这项将EPA供水记录与患者数据联系起来的全国性分析表明,即使是美国社区供水系统中铅含量处于低水平,但也与晚期肾病患者较低的血红蛋白水平以及较高的ESA使用率相关。
尽管肾病患者可能特别容易受到与铅接触相关的不良健康效应的影响,但饮用水中常见的铅含量是否与ESKD患者的不良结果相关尚未明确。
近日,肾脏病领域权威杂志Journal of the American Society of Nephrology上发表一篇研究文章,该研究旨在调查社区供水系统中的铅含量与ESKD患者血红蛋白浓度和促红细胞生成素刺激剂(ESA)使用之间的关联。研究人员合并了来自环境保护署(EPA)安全饮用水信息系统的数据(根据居住城市,记录了透析开始前5年内社区供水系统中平均90%的铅浓度数据)以及来自美国肾脏数据系统的患者数据。
在美国2005年至2017年期间开始透析的597968名患者中,社区供水系统中可检测到铅的城市ESKD患者血红蛋白浓度显著降低,ESA使用量增加。208912名患者的研究结果与ESKD治疗第一个月的数据相似,铅浓度每升高0.01mg/L,血红蛋白较低且ESA使用率较高。在铅水平强制采取监管行动达到EPA阈值(0.015mg/L)以下仍观察到这一关联。研究人员还观察到了环境因素的不公平现象,发现与白人相比,黑人的供水系统中铅水平更高,随着时间的推移下降速度更慢。
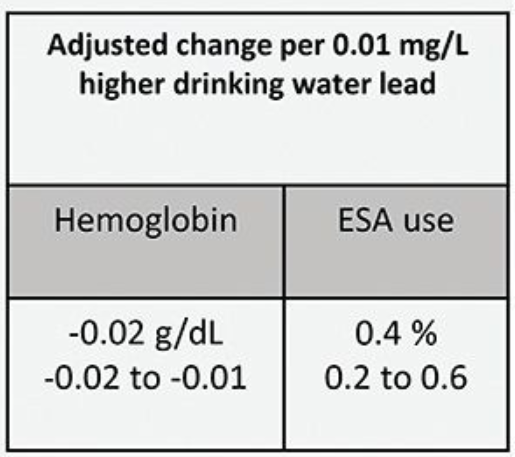
由此可见,这项将EPA供水记录与患者数据联系起来的全国性分析表明,即使是美国社区供水系统中铅含量处于低水平,但也与晚期肾病患者较低的血红蛋白水平以及较高的ESA使用率相关。
原始出处:
John Danziger,et al.Associations of Community Water Lead Concentrations with Hemoglobin Concentrations and Erythropoietin-Stimulating Agent Use among Patients with Advanced CKD.JASN,2021.https://jasn.asnjournals.org/content/early/2021/07/15/ASN.2020091281
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#ASN#
32
#CKD患者#
50
#社区#
26
#浓度#
29
理学物理领域
62
理工学物理
70
学了
0