Modern Pathology:睾丸非精原生殖细胞肿瘤转移的病理预测因素
2020-12-31 AlexYang MedSci原创
睾丸非精原生殖细胞肿瘤患者转移性疾病的病理风险因素存在争议。睾丸癌的肿瘤-结节-转移(TNM)分类第八版包括了国际抗癌联盟(UICC)和美国癌症联合委员会(AJCC)的不同版本。
睾丸非精原生殖细胞肿瘤患者转移性疾病的病理风险因素存在争议。睾丸癌的肿瘤-结节-转移(TNM)分类第八版包括了国际抗癌联盟(UICC)和美国癌症联合委员会(AJCC)的不同版本。
最近,有研究人员参照了上述两种分类法,调查了219名非精原生殖细胞肿瘤转移性疾病的病理预测因素。研究人员评估了年龄、肿瘤大小、胚胎癌的百分比、淋巴血管侵袭、基质性睾丸、门静脉软组织、附睾、精索、鞘膜以及精索边缘的肿瘤,并分析了与临床阶段的相关性。结果表明,219例NSGCT病例中,151例(69%)为临床I期,68例(31%)为临床II/III期。单变量分析中,肿瘤大小(P=0.028)、胚胎癌百分比(P=0.004)、淋巴血管侵袭(P=0.001)、睾丸基质侵袭(P=0.001)、门静脉软组织侵袭(P=0. 010)、附睾侵袭(P=0.010)、精索直接侵袭(P=0.001)、精索边缘肿瘤(P=0.009)均与与较高的临床分期有关。在多变量分析中,淋巴管侵袭(P=0.003)、肿瘤大小(P=0.005)、胚胎癌百分比(P=0.005)、睾丸基质侵袭(P=0.008)仍然显著。6cm肿瘤大小和70%胚胎癌百分比是显著的分界值。
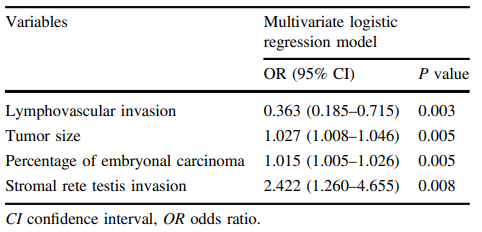
多变量回归模型表明的更高临床分期的潜在预测因子
最后,研究人员指出,除了淋巴血管侵袭外,睾丸基质侵袭、肿瘤大小和胚胎癌百分比都是转移性疾病出现的强有力的预测因素,且在未来的任何TNM修订中应考虑将其纳入。更多的是,他们的结果支持AJCC TNM第八版的修改,因为附睾和门静脉软组织的侵袭都有单变量显著性。
原始出处:
Glenda Scandura, Thomas Wagner, Luis Beltran et al. Pathological predictors of metastatic disease in testicular non-seminomatous germ cell tumors: which tumor-node-metastasis staging system? Modern Pathology. Dec 2020
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














有卵黄囊性的吗
57
#Pathol#
44
#预测因素#
45
#肿瘤转移#
67
#睾丸#
61
#生殖细胞#
52
#生殖细胞肿瘤#
46