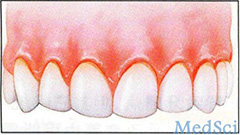
J Periodontol:牙周疾病可影响2型糖尿病患者的糖化血红蛋白的水平
2016-08-30 MedSci MedSci原创
关于长期牙周感染对糖尿病控制的研究甚少。本次回顾性队列研究旨在评估牙周状况对2型糖尿病患者的糖化血红蛋白水平的影响。 研究共纳入了8名2型糖尿病患者(年龄在56.0±8.9岁)。患者不吸烟,年龄≥40岁,使用抗糖尿病药物。从病历中获得患者的人口统计学信息,既往史和糖化血红蛋白的水平。记录探诊深度和临床附着丧失。 对患者进行两次检查,两次时间点平均间隔38.6±6.6个月。基线时诊断为重
关于长期牙周感染对糖尿病控制的研究甚少。本次回顾性队列研究旨在评估牙周状况对2型糖尿病患者的糖化血红蛋白水平的影响。
研究共纳入了8名2型糖尿病患者(年龄在56.0±8.9岁)。患者不吸烟,年龄≥40岁,使用抗糖尿病药物。从病历中获得患者的人口统计学信息,既往史和糖化血红蛋白的水平。记录探诊深度和临床附着丧失。
对患者进行两次检查,两次时间点平均间隔38.6±6.6个月。基线时诊断为重度牙周炎的患者,至少一颗牙有≥2MM的附着丧失(2.24%,95%可信区间为1.56-2.91),男性(2.75%,95%可信区间为1.72-3.78),以及基线糖化血红蛋白<6.5%(3.08%,95%可信区间为2.47-3.69)的患者,随时间推移其糖化血红蛋白水平的增加具有显著的统计学意义(2.32%,95%可信区间为1.50-3.15)。校正基线糖化血红蛋白的水平后,对于重度牙周炎患者以及附着丧失增加的患者其糖化血红蛋白的水平仍增加显著,分别为0.85%和0.9%。校正性别和糖化血红蛋白的水平后,附着丧失增加仍与糖化血红蛋白的水平增加(0.84%)显著相关,差异具有统计学意义。
总而言之,牙周炎的进展与2型糖尿病患者糖化血红蛋白的水平增加有关。这些危险因素的识别表明通过牙周治疗消除牙周感染或能够改善2型糖尿病的血糖控制。
原始出处:
COSTA KL, TABOZA ZA, ET AL., The Influence of Periodontal Disease on Changes of Glycated Hemoglobin Levels in Type 2 Diabetics: a Retrospective Cohort Study. J Periodontol. 2016 Aug 26:1-13.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#PE#
29
好文章,受益
44
赞!好文待探究。
0
文章不错
58
很好,不错,以后会多学习
54
互相影响
48
学习了,好
22
#糖尿病患者#
20
#2型糖尿病患者#
27
#牙周疾病#
39