J Clin Oncol:贝伐珠单抗联合标准化疗用于广泛期SCLC一线治疗的疗效如何?
2017-04-29 Riesling 肿瘤资讯
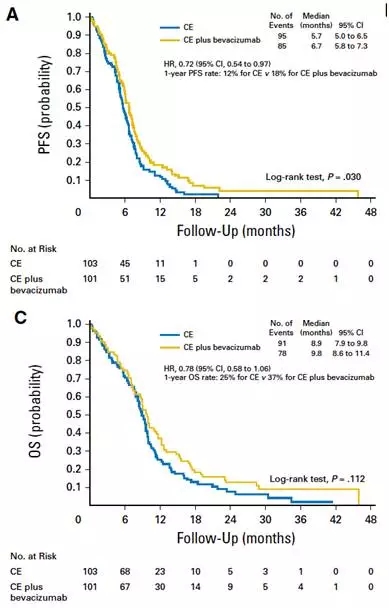
小细胞肺癌(SCLC)是一类侵袭性很强的肿瘤,因为肿瘤基因突变谱异常复杂,一直没有发现有意义的治疗靶点,几十年来,SCLC的治疗上仍然停留在放化疗为主的传统时代。探寻潜在的治疗靶点迫在眉睫。贝伐珠单抗,人源化的靶向VEGF单抗,目前已获批用于非小细胞肺癌、乳腺癌、结直肠癌、肾癌和卵巢癌。既往的II期研究中,贝伐珠单抗用于SCLC初见成效。FARM6PMFJM是一个随机多中心III期临床研究,旨在探

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#贝伐珠#
0
#Oncol#
24
#标准化疗#
50
#标准化#
27
#贝伐#
22
希望中国式的研究越来越有前景
54
希望能研究出其他活疗小细胞肺癌的免疫治疗药物,且能延缓复发。
68
好研究 方向不错^_^
72
学习了,谢谢分享
62
学习了很有用
66