半脱位年轻恒牙牙髓存活1例
2019-07-17 李红 牙体牙髓牙周病学杂志
患儿男,7岁。2016-02因上前牙外伤3h于我院儿童口腔科就诊。检查:11牙冠完整,伸长,根颈1/3暴露,松动Ⅲ°,牙龈缘渗血。21牙冠完整,松动Ⅰ°,牙龈缘渗血。
1.病例报告
患儿男,7岁。2016-02因上前牙外伤3h于我院儿童口腔科就诊。检查:11牙冠完整,伸长,根颈1/3暴露,松动Ⅲ°,牙龈缘渗血。21牙冠完整,松动Ⅰ°,牙龈缘渗血。
X线片示:11根尖区牙周膜间隙增宽,牙根发育7期(Nolla分期),未见明显根折线;21根尖区牙周间隙稍增宽,未见明显根折线(图1a)。诊断:11半脱位;21亚脱位。治疗:局麻下11手法根方复位,用正畸结扎丝(0.025mm×5股)+复合树脂对54、53、11、21、63、64行夹板固定(图1b),然后制取上颌模型及全牙列牙合垫,消除咬合创伤。2周后复查,拆除夹板并停戴全牙列牙合垫,11、21无松动,冷、热诊同对照牙。3个月后复查,11、12无明显不适,冷热诊较对照牙敏感,无松动,叩(-),牙龈未见异常;X线片示:11、12牙根继续发育,根尖周未见明显异常(图1c)。12个月后复查:11、21无不适,冷热诊同对照牙,无松动,叩(-),牙龈未见明显异常;X线片示:11根管壁增厚,管腔明显缩窄,根尖孔聚拢倾向,牙根长度明显增加(图1d)。22个月后复查:11、21无不适,牙冠颜色正常,冷热诊同对照牙,无松动,叩(-),牙龈未见明显异常;X线片示:11根尖孔聚拢,牙根长度同邻牙(图1e)。
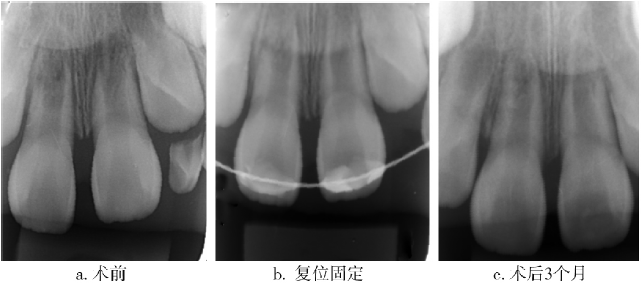
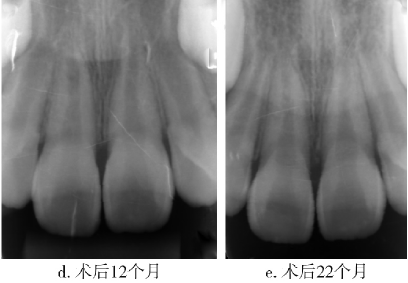
图1 11、21术前及术后X线片。
2.讨论
年轻恒牙外伤多发生于7~9岁儿童,占恒牙外伤的50%~70%。在牙根未完全形成时,外伤牙的松动、移位、脱出较常见,主要原因为刚萌出牙齿的牙根未完全形成,其牙槽骨、牙周膜等支持组织较脆弱,受外力后容易从牙槽骨中脱出。半脱位牙的治疗原则是及时复位并固定患牙,同时消除咬合创伤,严密观察牙髓状态的转归。脱位性损伤的牙齿,常伴有牙周膜充血、撕裂、出血;在愈合过程中,患牙要保持一定的生理动度,否则易发生牙齿固连。因此,在脱位牙固定时应采用弹性固定。
目前,常用的外伤牙固定方式有钢丝-树脂夹板固定术、正畸托槽+钢丝固定术、全牙列牙合垫固定术、钢丝结扎牙弓夹板固定术、牙外伤钛板固定术、树脂夹板固定术、超强纤维树脂夹板固定术等。本病例选择了多股结扎丝+复合树脂构成的夹板固定,同时为消除咬合创伤,配合使用全牙列牙合垫。
原始出处:
李红.半脱位年轻恒牙牙髓存活1例[J].牙体牙髓牙周病学杂志,2018(08):496+465.
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#牙髓#
38
#脱位#
43
#恒牙#
0