JNCCN: 循环肿瘤DNA(ctDNA)应用于去势抵抗的转移性前列腺癌临床管理:多中心真实世界研究结果
2021-05-17 yd2015 MedSci原创
使用ctDNA阐述了中国人群去势抵抗的转移性前列腺癌(mCRPC)不同治疗方式下的基因组改变谱。并且发现CDK12基因改变在中国人群中明显升高。多因素分析,CDK12 缺失,TP53 or RB1 缺
去势抵抗的转移性前列腺癌(mCRPC)仍不能治愈,尽管出现了较多的治疗措施,比如新的内分泌治疗,紫杉类药物以及PARP抑制剂。基因组学发现mCRPC中伴有DNA损伤修复基因(DDR)、雄激素受体(AR)基因、肿瘤抑制基因TP53和RB1的改变。有研究发现这些基因的改变跟mCRPC的治疗临床预后有关。但是这些重要的进展基本都是基于西方人群的基因组改变,中国人群跟西方人群在mCRPC中基因组改变是不是有区别仍不得而知,这些基因的改变是否也能预测中国人群mCRPC不同治疗方式的临床预后呢?
由于mCRPC骨转移和其他转移瘤的组织获得困难。循环肿瘤DNA(ctDNA)是一种较好的组织来源,而且能够兼容不同时间点的多种标本以及精确的计算肿瘤的异质性。已有研究报道了mCRPC患者之间以及肿瘤内存在肿瘤异质性。另外,mCRPC的基因组改变是动态的,随着治疗的不同有改变,这就说明肿瘤不同阶段治疗伴有多种多样的分子特征。
因此,针对上诉问题,近期来自中国多个中心的研究团队在Journal of the National Comprehensive Cancer Network (JNCCN)杂志上发表相关研究成果,在中国人群中的去势抵抗的转移性前列腺癌(mCRPC)患者,应用循环肿瘤DNA(ctDNA)测序描述DNA损伤修复基因的改变以及其他重要的驱动基因,并且评估基因的遗传学改变跟多种治疗的临床预后的关系,特别是DNA损伤修复基因。

该研究是一项多中心真实世界的研究。纳入了来自2017年12月至2019年12月8家研究中心的共292例mCRPC患者。获得了306份ctDNA标本。根据血液标本收集前的治疗分类时可分为:A 组(无治疗)为93 (30.4%), B组 (mCRPC一线治疗后)为132 (43.1%), and, 和C组(mCRPC二线或以上治疗后) 为81 (26.5%)。根据血液标本收集后的治疗分类时可分为:阿比特龙(n=58), 多西他赛 (n=66), 多西他赛后铂类为基础的化疗(n=19), 奥拉帕尼(n=27), and 其他治疗 (n=136)。
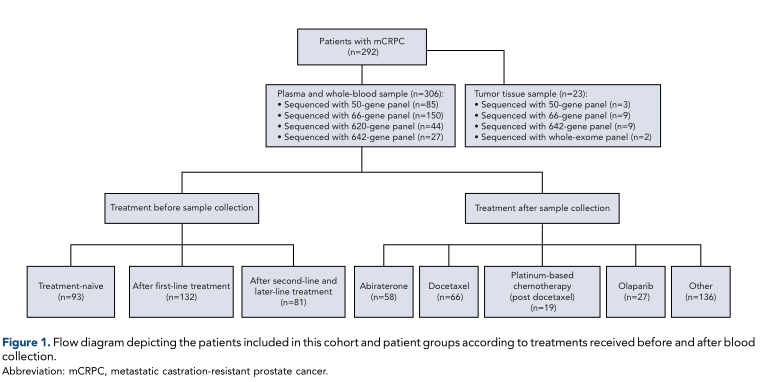
不同分组情况
研究数据表明,23例进行血液ctDNA检测的患者同时也有相应的组织进行检测,5例患者血液ctDNA和组织中都没有检测到突变。总的来说,33 of 36 (91.7%) 突变发生在血液ctDNA和组织检测中是一致的。
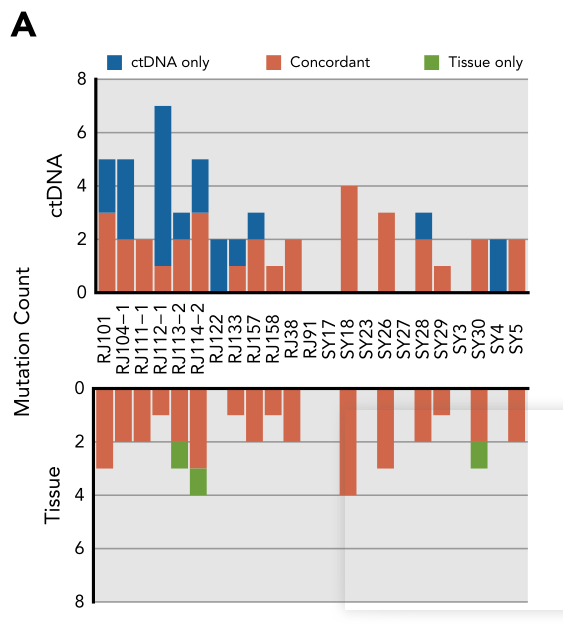
血液与组织基因检测度较一致
最常见的基因组改变为AR (34.6%), TP53 (19.5%), CDK12 (15.4%), BRCA2 (13%), and RB1 (5.8%)。AR基因改变在A组中为21.5%,B组为37.1%和C组中为46.9%,有统计学差异(P=0.001)。同样,TP53基因改变在C组中(24.7%)较A组(12.9%)明显升高(P=0.035)。并且,中国人群CDK12的改变(15.4%)明显高于西方人群(5%–7%)。
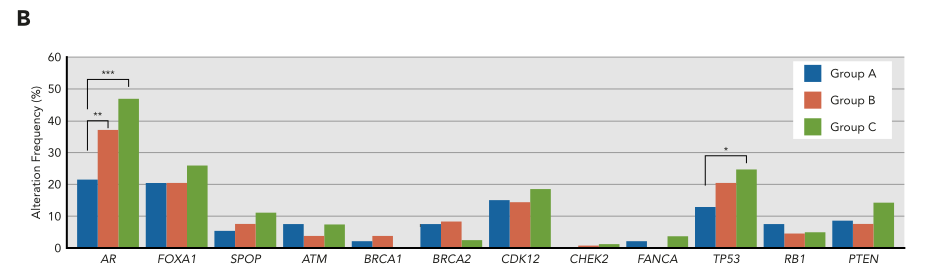
中国人群常见基因改变谱
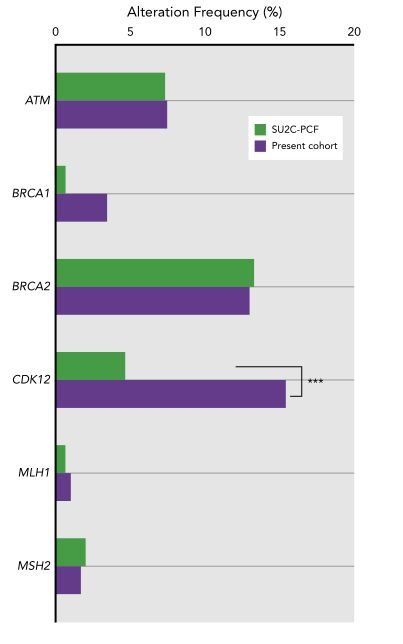
中国人群跟西方人群常见基因对比
58例阿比特龙治疗前收集ctDNA分析的患者中,12周时PSA下降大于50%在27例患者中出现(46.55%)。阿比特龙治疗后携带CDK12缺失的患者PFS更短(1.6 vs 10.4个月; P=0.001)。同样,阿比特龙治疗后携带TP53或RB1缺失的患者PFS更短(2.0 vs 11个月; P=0.001)。AR基因获得改变的患者PFS为3.0个月,而没有AR基因获得的患者PFS为10.4个月,两组有统计学差异((P=0.007)。但是AR基因突变与否并不影响阿比特龙治疗的PFS。

阿比特龙治疗疗效
66例只有多西他赛治疗前收集ctDNA分析的患者中,12周时PSA下降大于50%在29例患者中出现(43.94%)。CDK12, BRCA2, 或 ATM 基因缺失并不影响多西他赛治疗的PFS。携带TP53或RB1缺失的患者较没有缺失的患者PFS更短(4.8 vs 8.0个月;P=0.019)。而AR基因获得的患者较没有AR基因获得改变的患者中位PFS更短(5.0 vs 8.0个月;P=0.012)。
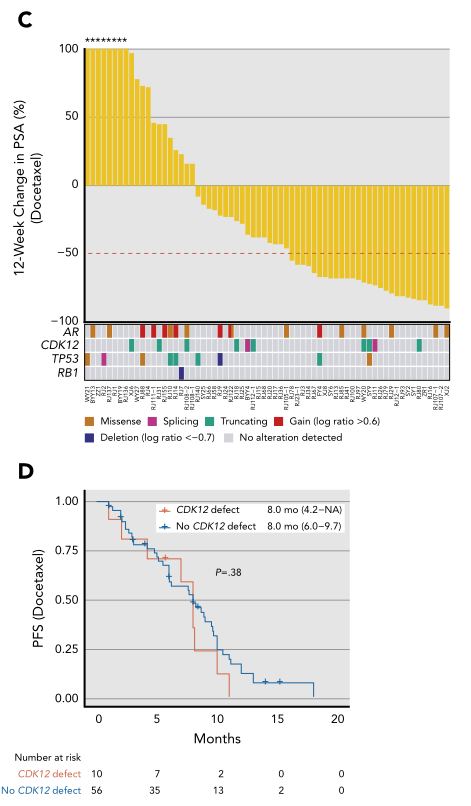
多西他赛治疗疗效
携带BRCA2缺失改变的患者对铂类为基础的化疗以及PARP抑制剂有良好的应答。多因素分析,CDK12 缺失 (HR=19.587; 95%CI, 3.788–101.278; P=0.001), TP53 or RB1 缺失 (HR=4.727; 95% CI, 1.554–14.383; P=0.006)是阿比特龙治疗的独立危险因素。而TP53 or RB1 缺失 (HR= 2.805; 95%CI,1.130–6.965;P=0.026)是多西他赛治疗的独立危险因素。
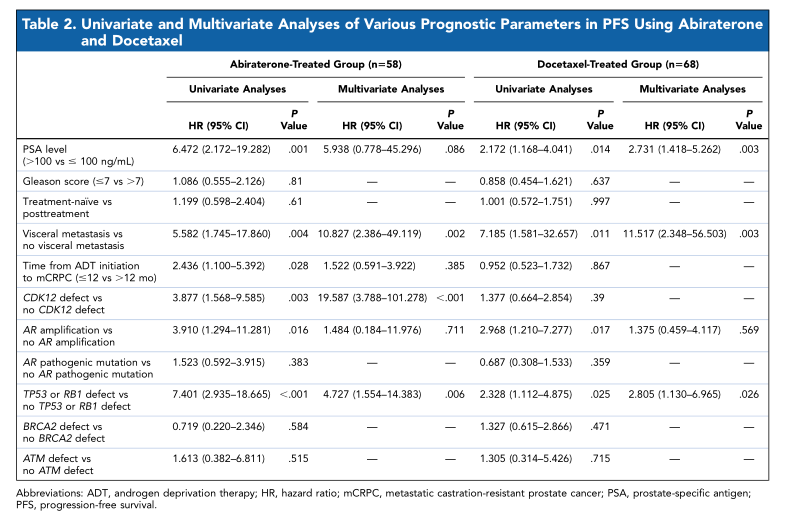
多因素分析阿比特龙和多西他赛的危险因素
综上,使用ctDNA阐述了中国人群去势抵抗的转移性前列腺癌(mCRPC)不同治疗方式下的基因组改变谱。并且发现CDK12基因改变在中国人群中明显升高。多因素分析,CDK12 缺失,TP53 or RB1 缺失是阿比特龙治疗的独立危险因素, TP53 or RB1 缺失则是多西他赛治疗的独立危险因素。
原始出处:
Baijun Dong, Liancheng Fan, Bin Yang MD, et al. Use of Circulating Tumor DNA for the Clinical Management of Metastatic Castration-Resistant Prostate Cancer: A Multicenter, Real-World Study. J Natl Compr Canc Netw. 2021 May 14;1-10. doi: 10.6004/jnccn.2020.7663. Online ahead of print.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言

















#研究结果#
33
#多中心#
30
#真实世界#
36
#NCCN#
38
#转移性#
40
#转移性前列腺癌#
46
#循环肿瘤DNA#
42
#临床管理#
35
学习
53
啊哈,学到了
69