从心电图如何快速诊断特发性室性心动过速?
2017-09-28 佚名 Medicalxpress
男性患者,13岁,反复阵发性心悸1年。入院后行心电图,因患者无器质性心脏病且室速反复发作诊断为左室特发性室速。此病临床特点是什么?心电图表现有哪些?详见以下病例——
【示教病例】
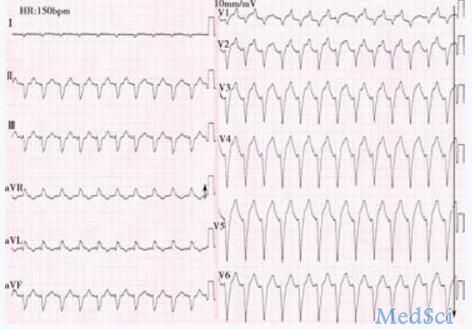
1.患者男性,13岁,反复阵发性心悸1年,再发1小时。行心电图检查(图5-4-14)。
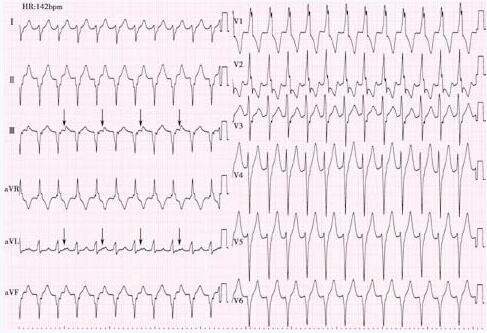 图5-4-14 心电图 心电图表现为右束支阻滞图形的宽QRS波心动过速,aVR导联呈高R型,Ⅰ、Ⅱ、Ⅲ导联波均向下,心电轴极度右偏。部分导联ST-T 呈2∶1交替,Ⅲ、aVL导联尤其明显,是室房2∶1逆传产生的逆行P波重叠于ST-T交界处所致(箭头所示)。心电图诊断:阵发性室性心动过速(结合患者无器质性心脏病,室速反复发作,临床诊断左室特发性室速)
图5-4-14 心电图 心电图表现为右束支阻滞图形的宽QRS波心动过速,aVR导联呈高R型,Ⅰ、Ⅱ、Ⅲ导联波均向下,心电轴极度右偏。部分导联ST-T 呈2∶1交替,Ⅲ、aVL导联尤其明显,是室房2∶1逆传产生的逆行P波重叠于ST-T交界处所致(箭头所示)。心电图诊断:阵发性室性心动过速(结合患者无器质性心脏病,室速反复发作,临床诊断左室特发性室速)【相关知识点】
1. 特发性室性心动过速(idiopatic ventricular tachycardia,IVT)的临床特点
特发性室速是指发生于无器质性(“结构正常”的心脏)心脏病患者的室性心动过速。这里所谓结构正常的心脏是指经过临床查体和现有检查方法均未发现心脏结构异常的证据,并排除代谢因素、离子通道疾病等,而只表现为室速。特发性室性心动过速一般为单形性室速,多呈阵发性发作,发作时血流动力学大多稳定,预后一般良好,极少数有晕厥和猝死的危险,可经导管射频消融术根治。
2. 特发性室速心电图表现
根据不同起源部位,可大致分为右室特发性室性心动过速和左室特发性室性心动过速。不同部位特发性室速不仅具有各自特征性心电图表现,同时还具有各自的临床特点。
(1) 右室特发性室性心动过速:主要起源于右室流出道,少数见于右室流入道、右室心尖部及右室前壁等部位。多在青壮年起病,体力活动或情绪应激可诱发,呈持续性或反复非持续性单形性室性心动过速,症状多轻微,对腺苷敏感,迷走神经兴奋、ATP、维拉帕米和β受体阻滞药对部分患者有治疗作用,普罗帕酮可有效防治室性心动过速的发作。右室不同部位起源的心电图表现如下:
(2) 左室特发性室性心动过速:多见于青壮年男性(男女比例约3∶1),运动和异丙肾上腺素易诱发,对维拉帕米敏感(部分对腺苷敏感),故又称维拉帕米敏感性室性心动过速。多数起源于左室间隔部,又以后中间隔的左后分支区域最多见,故又称分支性室性心动过速,少数起源于左室流出道等其他部位。左室不同部位起源的心电图表现如下:
【实战演练】
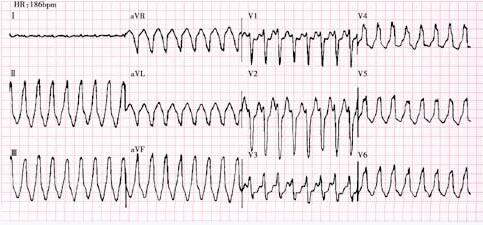
患者女性,28岁,阵发性心悸30分钟。行心电图检查(图5-4-15)。
【复习题及答案解析】
1. 下列有关左室特发性室性心动过速的描述,错误的是
1. 左室特发性室性心动过速(又称分支型或维拉帕米敏感性室性心动过速),多数起源于左室间隔部(少数起源于左室流出道等其他部位),心电图特征性表现为V1导联呈右束支阻滞图形,对维拉帕米敏感(部分对腺苷敏感);该病多见于青壮年男性,患者常有反复室性心动过速发作史,但一般无器质性心脏病变,对反复发作且有黑蒙、晕厥者应行射频消融术。答案:C
2. 特发性室性心动过速一般为单形性室性心动过速,多呈阵发性发作,发作时血流动力学大多稳定,预后一般良好,极少数有晕厥和猝死的危险。特发性室性心动过速可经导管射频消融术根治。值得注意的是,左室特发性室性心动过速多对维拉帕米敏感,心电图特征性表现为V1导联呈右束支阻滞图形;而右室特发性室性心动过速多对腺苷敏感,心电图表现为胸导联呈左束支阻滞图形。答案:D
《临床心电图精解》作者:廉姜芳 周建庆参编:叶明 葛世俊 巴艳娜 陈健页码:182-185出版:人民卫生出版社
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
相关资讯
急诊出诊的10个“陷阱”,你掉过几个?
急诊出诊时,我们会碰到很多的缓慢性心律失常患者,可能是良性的窦缓,也可能是“恶性”的三度,不同患者需要不同处理,处理恰当,可使患者迅速得到合理诊治,处理不当,轻者延误诊治,重者可危及患者生命。
3种心律不齐差别大,一不小心就会错!
很多人都有心慌的经历,这时候临床检查往往就会显示窦性心律不齐的诊断。心律不齐分为窦性心律失常、期前收缩和阵发性心动过速三种,每种心电图的意义都不相同。窦性心律不齐的原因是什么?窦房结释放出的激动频率不规则会导致心率显着快慢不均匀而引起的心律失常,称为窦性心律不齐。根据病因的不同,临床上将窦性心律不齐分为呼吸性窦性心律不齐、非呼吸性窦性心律不齐、窦房结内游走性节律、与心室收缩排血有关的窦性心律不齐、
逢胸话急:注意不典型胸痛
虽然患者一开始误认为自己是胃肠道问题,并出现干呕不适。但问诊时明确有左上肢牵涉痛,伴有大汗淋漓,因怀疑患者为急性冠脉综合征。需要就诊后立即检查心电图。该患者心电图明确提示ST段抬高型心肌梗死。结合患者胸痛表现,可不等心肌损伤标志物检查结果即可考虑冠脉造影。但需要注意患者血常规、凝血指标和肾功能情况。
让病人做个检查,医生就摊上大事了?
看个小病医生也让你做心电图,这就摊上大事了?
心电图诊断致心律失常性右室心肌病 表现和注意事项有哪些?
本例患者反复胸闷、心悸十余年,经心电图诊断为致心律失常性右室心肌病。其心电图表现有哪些?Fontaine导联描记方法有什么优势?ε波的临床意义是什么?这些问题将在下文详细解答。
心电图也是会骗人的,你知道吗?
心电图是通过仪器从体表记录心电活动的变化图,从而推测心脏疾病。既然是推测,就有可能出错,比如急性心肌梗死。临床偶尔会遇见心电图表现虽然酷似心梗,但并不是心梗,需鉴别。小编查阅相关资料,总结可能发生“假心梗”的疾病,并将其按发生机制分别整理于下。











#特发性#
46
#室性心动过速#
43
#心动过速#
29
学习
62
学习了.要是多点视频就好
64