Biomed Res Int:ERAP1基因多态性与银屑病易感性之间的关系
2021-10-30 MedSci原创 MedSci原创
银屑病是一种常见的慢性炎症性疾病,全世界约有2%-3%的人患有银屑病,在西方国家发病率更高。近几十年来,强大的全基因组关联研究和许多其他候选基因方法已经确定了许多与银屑病风险相关的基因。内质网氨肽酶1
银屑病是一种常见的慢性炎症性疾病,全世界约有2%-3%的人患有银屑病,在西方国家发病率更高。近几十年来,强大的全基因组关联研究和许多其他候选基因方法已经确定了许多与银屑病风险相关的基因。内质网氨肽酶1(ERAP1)属于氨肽酶M1家族,作为"分子统治者"发挥着核心作用,在抗原肽加载到HLA-I分子上以在内质网中呈现抗原之前,对抗原肽的N端进行蛋白分解。ERAP1属于M1锌金属肽酶的催产酶亚群,具有49%的序列相似性,并能形成异质体。人类的ERAP1基因在短臂染色体5q15的167Kb区域内编码,方向相反,可能,它们有两个共同的调节元件。ERAP1基因的多态性可能影响对银屑病的易感性。近日,发表于Biomed Res Int的一项荟萃分析探讨了内质网氨基肽酶1(ERAP1)基因多态性与银屑病的关系。
研究人员检索了2019年12月25日之前,PubMed、中国国家知识基础设施(CNKI)、Embase、Web of Science和Cochrane图书馆五个数据库收录的相关研究。使用纽卡斯尔-渥太华量表(NOS)评估纳入研究的质量。采用PRISMA进行了Meta分析。
结果,研究人员共纳入9个病例对照研究,包括4858个银屑病患者和10542个健康对照者。评估了ERAP1基因多态性的三个位点(rs26653、rs30187和rs27524)。分析结果显示,rs26653多态性与银屑病风险之间没有明显的关联(C与G,OR = 1.01,95% CI: 0.80-1.28,P = 0.93)。然而,rs30187多态性与银屑病易感性密切相关(T vs. C,OR = 1.23,95% CI:1.15-1.32,P < 0.00001),rs27524多态性与银屑病易感性密切相关(A vs. G,OR = 1.17,95% CI:1.09-1.25,P < 0.00001)。但是,由于rs27044、rs151823、rs2248374和rs2910686的数据不足,研究人员只对其进行了系统回顾。
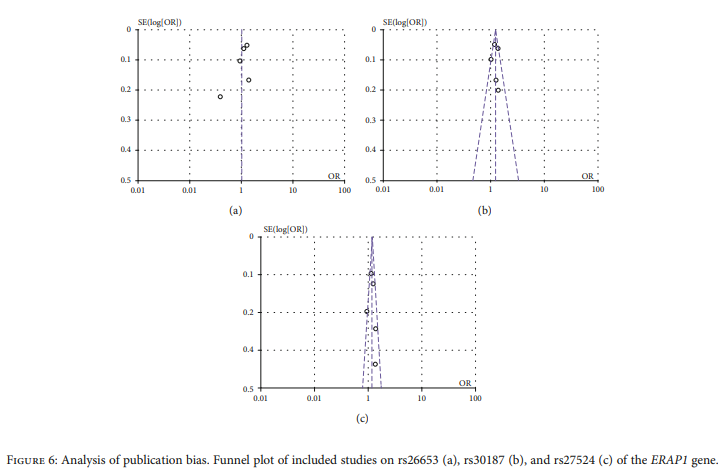
综上所述,该研究结果表明,ERAP1的rs30187(C/T)和rs27524(G/A)多态性与银屑病的风险增加有关。然而,rs26653(G/C)多态性与银屑病风险之间没有观察到明显的关联。
原始出处:
Xiujuan Wu, Zongfeng Zhao. Associations between ERAP1 Gene Polymorphisms and Psoriasis Susceptibility: A Meta-Analysis of Case-Control Studies. Biomed Res Int. 2021 Aug 2;2021:5515868. doi: 10.1155/2021/5515868.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#RAP1#
52
#Bio#
28
#ERA#
41
#易感性#
32
#Med#
27
#多态性#
40