PHILIPS每日一例:肾窦微小动静脉畸形(瘘)1例
2022-09-09 放射沙龙 中外健康文摘
肾动脉畸形(rAVM)和肾动静脉瘘(rAVF)在临床上较少见,确诊病例在临床上的治疗方案并不复杂,对其准确诊断是影像诊断的主要难题。
肾动静脉异常交通包括肾动脉畸形(rAVM)和肾动静脉瘘(rAVF)在临床上较少见,主要以肉眼血尿为首发症状,微小病灶超声检查及常规CT平扫加增强可以无异常发现。近期我院收治1病例,首次常规增强CT检查以肾窦移行细胞癌误诊,后经双动脉期扫描检查并手术,术后病理证实为肾窦微小动静脉畸形。现结合文献资料就该病认识总结如下:
1.临床资料
女,65岁,反复血尿3年,肉眼血尿4月,尿频尿急尿痛1天入院,入院前3年患者出现不明原因的尿血,血尿为淡红色,伴尿频、尿急、尿痛,同时自觉左侧腰部酸痛不适,在当地医院诊断为“尿路感染”,予抗感染、止血、支持对症治疗后缓解,此后上述症状反复发作,入院前一天再次发作,以“血尿待诊”入住泌尿科。
入院后行彩超检查提示:双肾轮廓清晰,形态大小正常,实质回声均匀,皮髓质分界清楚,集合系统不分离;膀胱输尿管未见异常,膀胱内尿液欠清,建议查尿Rt。辅查尿Rt镜检:红细胞计数12854个(0~8个/ul)白细胞总数189个(0~8个/ul)尿干化学项目:蛋白质(pro)>3.0,亚硝酸盐(NIT)+、隐血(BLD)200,白细胞(BWC)125,维生素C(Vc)2.8;尿素氮4.22mmol/L,血肌酐62μmol/L,甘油三酯3.3mmol/L,总胆固醇16.2mmol/L,转氨酶62U/L,抗核抗体阴性,胸片未见异常。
诊断尿路感染,血尿。予抗感染,止血及支持治疗。同时行双肾、输尿管、膀胱CT平扫+增强扫描。螺旋CT,层厚5mm,螺距0.95;平扫+双动脉期+平衡期+10分钟延时扫描,左肾影稍显丰满,轮廓形态尚存,左肾下盏内见不规则混杂密度影,其内未见脂肪密度,无明显边界,增强早期不规则明显快速强化,呈条状及迂曲状,无边界,无包膜,左肾静脉早期快速显影,并跟左肾动脉同步显影;实质期及延迟扫描均可见动静脉显影同步。
CTV可见左肾下盏呈受压变形改变。右肾及双侧输尿管及膀胱显影好,无异常发现。VR及MIP重建:左肾门下于动脉早期可见异常显影血管团形成,肾动脉及肾静脉异常交通,同步显影。如图:图1、图2、图3、图4。

图1动脉早期轴位示:左肾窦点状、细线状血管影;
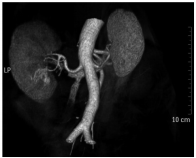
图2动脉早期VR重建示:左肾动、静脉早期快速显影,肾窦见迂曲血管团,动静脉异常交通支;

图3动脉晚期VR重建示:左肾窦迂曲血管团;

图4动脉晚期MIP重建示:左肾窦迂曲血管团及动静异常交通。
2.讨论
血管畸形为先天性或获得性血管异常而引起的疾病,先天性是由于胚胎芽内原始血管的发育障碍或发育异常所致,属非肿瘤样病变。传统的血管畸形分类多种多样,Mulliken等根据对各种血管瘤标本的内皮细胞进行体外培养后,并结合病变的临床表现、胚胎组织学和血流动力学特征,在细胞学的基础上将血管瘤的概念明确分为血管瘤和血管畸形两大类,又将血管畸形分成高流量和低流量两类。高流量血管畸形再分为动静脉瘘和动静脉畸形。
AVM由增粗的供血动脉、畸形血管团和迂曲扩张的引流静脉组成,供血动脉与引流静脉之间多为异常毛细血管床。AVM可发生于任何部位,以颅内、颜面和四肢部多见。其临床症状与解剖部位、大小和其引起的并发症相关。其中肾血管畸形相对少见,发病率低于0.04%,且临床上多无阳性体征或仅有无痛性血尿,在常规检查中不易发现。
rAVM通常以不明原因无痛性大量血尿为首要表现,通常以DSA为首选的诊断方法,近年来随着医学影像及CT扫描及后处理技术的飞速发展,早期双动脉期扫描,应用CTA后处理技术,该病的诊断及治疗水平得到一定提高,实现了无创早期快速检查。
3.总结
肾动脉造影对肾血管畸形的诊断重要性不言而喻。造影可显示供血动脉增粗,成团的迂曲血管,肾静脉早显,对于细小隐匿者,则需超选择性造影和多角度投照方可显示。在实际临床工作应用中,当出现相应临床症状时应用常见病及多发病不能得到合理解释时可以提示有微小肾动静脉畸形(瘘)的可能,此时遵循由简到繁的检查原则,可以再行肾脏CT增强检查时利用多排螺旋CT快速扫描的优势及特点,行双动脉期扫描。
扫描方法1,固定时间法:平扫、动脉早期(20~22s)、动脉晚期(30~35s)和门静脉期(60s)必要时加延时期(180~600s),该方法动脉早期及晚期时间均比肝动脉双期扫描推迟1~2秒;方法2,阈值触发技术,相对复杂,但准确率高,兴趣点选择降主动脉水平,延迟时间5s开始扫描,动脉早,晚期间隔10s。采用2mm层厚,1mm层间距容积扫描,利用VR,MIP及CTA等后处理技术,行肾动脉重建,多角度旋转观察,可以发现在动脉早期是畸形血管增粗的供血动脉及迂曲血管团,动脉晚期时可以发现同侧肾静脉显影,同步(或早于)肾髓质显影。
总之,肾动脉畸形(rAVM)和肾动静脉瘘(rAVF)在临床上较少见,确诊病例在临床上的治疗方案并不复杂,对其准确诊断是影像诊断的主要难题,在实际工作中应当给予相应的重视,通过适当调整检查方法可以提高该病的发现率及诊断准确率,并减少行DSA检查的痛苦及风险。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#期刊论坛##学习#
0
不错的文章
33
#静脉#
32
#动静脉畸形#
32
#畸形#
29
#iPS#
19