NEJM:经导管主动脉瓣植入后单药与双药抗血小板治疗比较
2020-10-09 MedSci原创 MedSci原创
在接受TAVI且无口服抗凝适应症的患者中,仅阿司匹林治疗3个月出血发生率以及出血或血栓栓塞复合事件发生率显著低于阿司匹林加氯吡格雷治疗。
对于没有长期抗凝指征的患者,单药与双药抗血小板治疗对经导管主动脉瓣植入术(TAVI)后出血和血栓栓塞事件的影响尚未明确。
近日,顶级医学期刊NEJM上发表了一篇研究文章,在这项随机对照试验中,研究人员将接受TAVI治疗且无长期抗凝指征的患者亚组按1:1的比例分配单独接受阿司匹林或阿司匹林加氯吡格雷治疗3个月。该研究两个主要结局是所有出血(包括轻度、重度和危及生命或致残性出血)和12个月内与手术无关的出血。大部分出血为TAVI穿刺部位出血,其被认为与手术无关。该研究两个次要结局是心血管原因、非手术相关出血、卒中或心肌梗死的死亡复合事件(次要结局1)和心血管原因、缺血性卒中或心肌梗死的死亡复合事件(次级结局2)。在1年时,两项结局依次进行非劣效性(非劣效性边际为7.5个百分点)和优势检验。
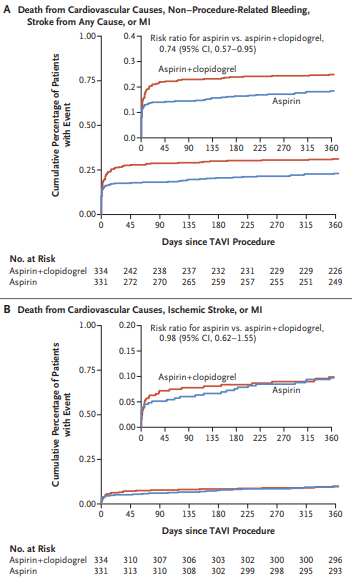
该研究总共有331例患者被分配接受阿司匹林治疗,而334例患者被分配接受阿司匹林加氯吡格雷治疗。仅接受阿司匹林受试者中有50例(15.1%)患者发生出血事件,接受阿司匹林加氯吡格雷的受试者中有89例患者(26.6%)发生出血事件(风险比为0.57;95%置信区间[CI]为0.42至0.77;P=0.001)。各组分别有50例患者(15.1%)和83例患者(24.9%)发生了与手术无关的出血(风险比为0.61;95%CI为0.44至0.83;P=0.005)。仅接受阿司匹林的76例患者(23.0%)和接受阿司匹林加氯吡格雷的104例患者(31.1%)发生了次要结局1(差异为-8.2个百分点;非劣效性95%CI为-14.9至-1.5;P<0.001 ;风险比为0.74;优势95%CI为0.57至0.95;P=0.04)。各组分别有32例患者(9.7%)和33例患者(9.9%)发生次要结局2(差异为-0.2个百分点;非劣效性95%CI为-4.7至4.3;P=0.004;风险比为0.98;优势95%CI为0.62至1.55;P=0.93)。在试验期间,分别有44例患者(13.3%)和32例(9.6%)接受了口服抗凝治疗。
由此可见,在接受TAVI且无口服抗凝适应症的患者中,仅阿司匹林治疗3个月出血发生率以及出血或血栓栓塞复合事件发生率显著低于阿司匹林加氯吡格雷治疗。
原始出处:
Jorn Brouwer,et al.Aspirin with or without Clopidogrel after Transcatheter Aortic-Valve Implantation.NEJM.2020.https://www.nejm.org/doi/full/10.1056/NEJMoa2017815
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#经导管主动脉瓣植入#
36
好文章
78
#主动脉瓣#
35
#主动脉#
40
#经导管#
45
#植入#
33
#治疗比较#
26
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
50