Lancet Oncol:癌症的预防性治疗要靠谱!
2017-08-08 王强 肿瘤资讯
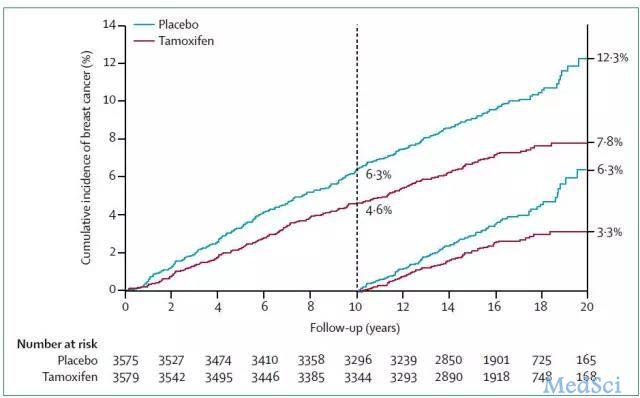
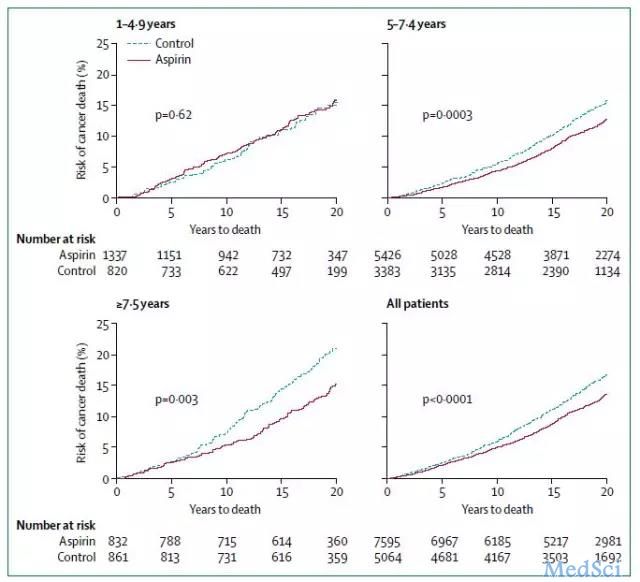
防癌措施多种多样,包括调整生活方式、通过筛查检出早期病变、积极干预癌变过程等。相比已得到确证的心血管疾病预防而言,癌症的预防性治疗尚处于早期阶段。本文即对具有有效证据的相关干预措施进行概述。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#预防性治疗#
0
#Oncol#
30
#靠谱#
25
#Lancet#
21
#预防性#
22
谢谢
54
谢谢
59
谢谢
56
谢谢
41
谢谢
41