BMC Musculoskelet Disord:应用Taylor空间框架治疗胫骨骨折的标记物-三维测量与传统X线测量
2022-09-20 医路坦克 MedSci原创
开放性胫骨骨折骨延迟愈合和骨不连在临床实践中较为常见。本研究的目的是提出一种新的MARKER-3D测量方法,并确定MARKER-3D测量方法与传统X线测量方法在TSF治疗中的复位结果的差异。
开放性胫骨骨折骨延迟愈合和骨不连在临床实践中较为常见。外固定架在这些问题的治疗中起着重要的作用,它为骨折愈合提供了有利的微环境,并在治疗骨不连、骨髓炎和其他疾病方面具有优势。然而,传统的伊利扎罗夫系统需要一个较长的学习过程。泰勒空间框架(TSF)是由Stewart平台和Ilizarov外固定器衍生而来的,由6根伸缩支柱连接的两个完整或不完整的环组成。TSF可以在不改变框架结构的情况下同时矫正空间变形,在骨科手术中得到了广泛的应用。
然而,TSF系统的参数需要在射线照片上手动测量,在传统的射线测量中存在主观误差。此外,轴向信息不能从二维X射线获得,通常通过体检来估计。上述缺点往往导致骨折对齐不良,导致更多的复位过程和治疗持续时间。此外,下肢对齐不良是膝骨性关节炎的独立危险因素,较好的对齐有利于功能重建。随着成像技术的发展,三维重建技术在医学上得到了广泛的应用。在骨折病例中,三维重建技术提供了传统X射线不能提供的轴向信息。
在以前的研究中,安装在环上的标记被引入到3D重建过程中。在本研究中,调整方案可以在自主开发的软件的帮助下自动生成,避免了人工测量可能存在的主观误差。本研究的目的是提出一种新的MARKER-3D测量方法,并确定MARKER-3D测量方法与传统X线测量方法在TSF治疗中的复位结果的差异,为今后旨在使TSF过程更有效的工作铺平道路。
方法:对2016年1月至2019年6月应用TSF治疗的41例胫骨骨折患者进行回顾性分析,其中MARKER-3D测量组(实验组)21例,传统X线测量组(对照组)20例。试验组在TSF上安装6个标记进行三维重建,以确定电子处方。对照组采用正位和侧位X线片进行常规参数测量。根据复位后的AP和侧位X线片,以冠状面和矢状面的残存移位畸形(RDD)和残角畸形(RAD)来评价疗效。
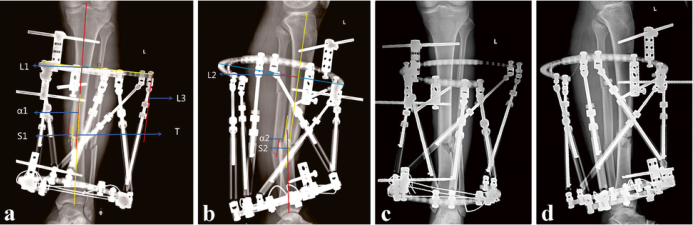
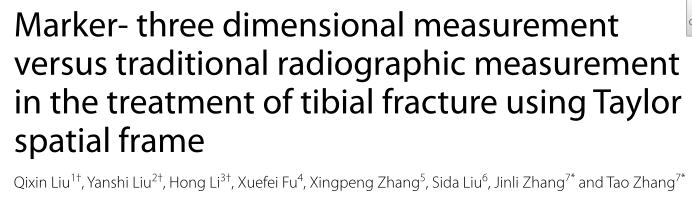
图1 胫骨骨折患者使用传统的放射测量方法进行TSF治疗的X线片。男性,33岁,左侧。AP视图中的测量变形参数。B侧位测量畸形参数。C缩小后的即时AP视图。还原后的直视侧位

图2 记号笔的组成

图3 三维重建模型。以骨折线为界,将重建的患肢骨模型分为近端和远端骨模型。模型近端(受影响肢体近端骨骼的3D模型)、模型远端(受影响肢体远端骨骼的3D模型)和模型参考(健康肢体骨骼的3D镜像模型)。模型框架(外固定架的三维模型)和模型标记球(标记球的三维模型)
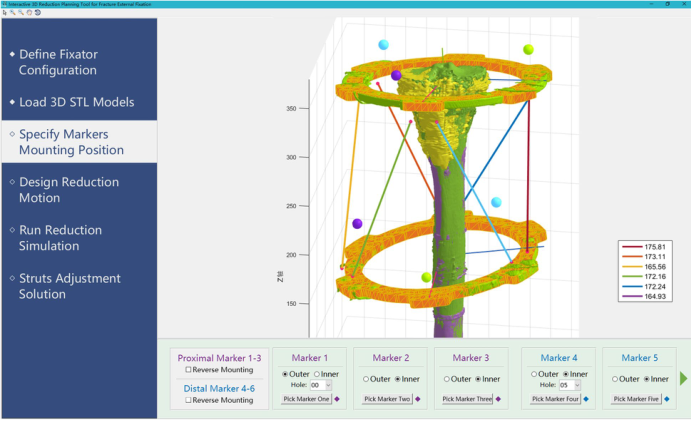
图4 3D还原软件界面
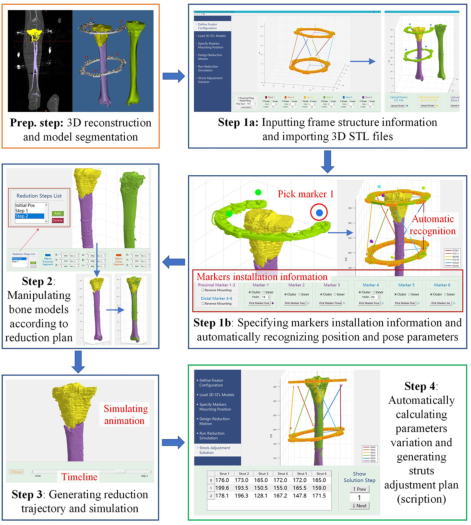
图5 标记器示意图-3D重建法
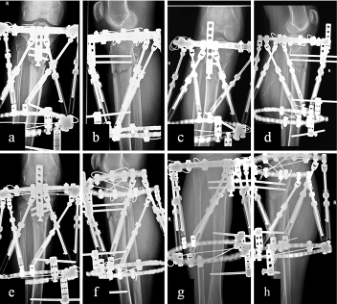
图6 胫骨骨折患者使用标记物-3D测量方法进行TSF治疗的X线片。男性,74岁,右侧。术后即刻切面及侧位观察。C、d复位后即刻切面及侧位片。术后1个月。三个月后手术后
结果:所有患者均获得功能恢复。观察组的残余RDD为0.5(0,1.72)mm,对照组为1.74(0.43,3.67)mm。观察组的残余RAD为0(0,1.25)°,对照组为1.25(0.62,1.95)°。侧位RDD试验组为0(0,1.22)mm,对照组为2.02(0,3.74)mm,RAD为0(0,0)°,对照组为1.42(0,1.93)°。两组间比较差异均有统计学意义(P=0.024,P=0.020;P=0.016,P=0.004)。
结论:本研究引入了一种标记物-3D测量方法来补充目前的TSF治疗。该方法避免了人工测量误差,提高了骨折复位的准确性,为骨愈合和功能康复提供了潜在的优势。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#BMC#
61
#标记物#
41
#Dis#
35
#Disord#
47
#胫骨骨折#
43
#X线#
42
#胫骨#
30