Nat Med:癌症耐药新机制
2018-02-14 Ruthy,Yui 转化医学网
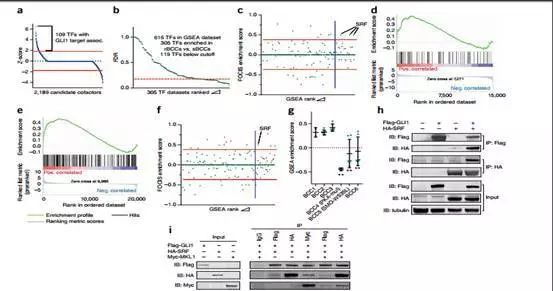
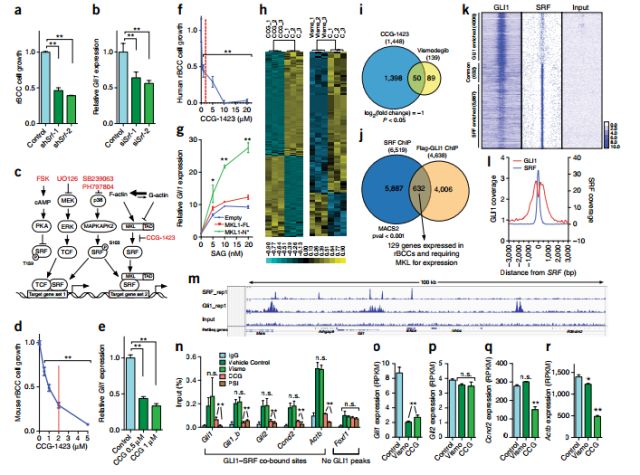
基底细胞癌(BCC)是最为常见的皮肤癌类型,基于它有较大的破坏性,又称侵袭性溃疡。这是一种严重破坏容貌的癌症,但较少危及生命。最新的一项研究表明,BCC肿瘤细胞中存在着一种 不依赖于基因突变的药物抵抗机制,使得许多的皮肤癌患者在诊断时即存在着耐药性。这项研究成果有利于对BCC患者进行更有效的治疗并为个人专项治疗提供理论基础。


本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Nat#
24
#癌症耐药#
25
不错.希望对各种肿瘤有帮助
47
#Med#
31
学习一下谢谢
0
阅
45
阅
50
阅
50
这种方法可能有利于BCC患者的治疗.同时能帮助研究人员制定更好的个性化治疗方案
25