JAMA Internal Medicine:乳腺癌左侧放疗及仰卧体位增加患者心血管疾病死亡风险
2013-11-04 佚名 丁香园
研究要点: 1.既往研究证实,乳腺癌后放疗可增加心血管疾病长期死亡率; 2.本研究发现,乳腺癌基础风险高、接受左侧放疗、放疗体位为仰卧位的女性,发生心血管事件风险率最高; 3.通过控制基础心血管疾病的危险因素、改善患者生活方式以及心血管病药物治疗,可减少乳腺癌放疗患者长期心血管疾病死亡率。 目前,许多研究证实,乳腺癌后放疗可增加心血管疾病长期死亡率。
研究要点:
1.既往研究证实,乳腺癌后放疗可增加心血管疾病长期死亡率;
2.本研究发现,乳腺癌基础风险高、接受左侧放疗、放疗体位为仰卧位的女性,发生心血管事件风险率最高;
3.通过控制基础心血管疾病的危险因素、改善患者生活方式以及心血管病药物治疗,可减少乳腺癌放疗患者长期心血管疾病死亡率。
目前,许多研究证实,乳腺癌后放疗可增加心血管疾病长期死亡率。但哪些患者、哪些放疗方式容易增加心血管疾病死亡率,目前仍缺乏报道。基于此,来自纽约哥伦比亚大学医学中心的David J博士等人进行了一项研究,研究结果在线发表于JAMA Internal Medicine杂志上。
本研究共纳入48名受试者,均为乳腺癌IIA级0期患者,这些患者于2005年在纽约大学肿瘤放疗科接受乳腺癌放疗。专家们比较了这些患者乳腺癌放疗与心血管病之间的关系,纳入因素包括心血管疾病用药、心血管疾病风险、左侧还是右侧接受放疗、放疗时的患者体位以及急性心血管事件。
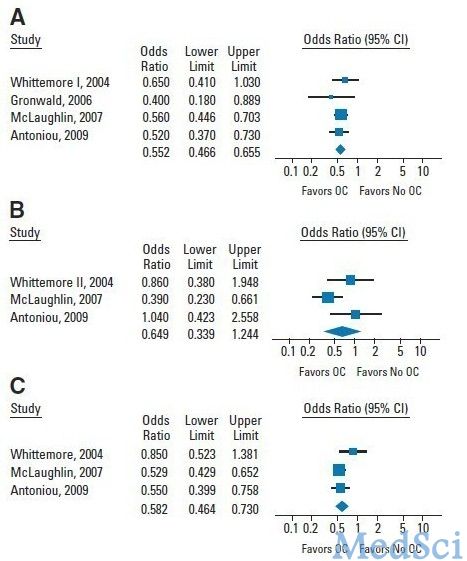
本项研究指出,乳腺癌基础风险高、接受左侧放疗、放疗体位为仰卧位的女性,发生心血管事件风险率最高,而乳腺癌基础风险低、接受右侧放疗女性,发生心血管事件风险率最低。对于左侧放疗患者,采取俯卧体位可减少心血管疾病用药及风险,而右侧放疗患者,由于心脏在放疗范围外,其心血管事件发生率与体位无明显相关。研究还指出,由于放疗对心血管疾病的影响是多因素的,并且心血管病的基础风险越高,放疗的绝对风险越高,因此,通过控制心血管疾病的危险因素(如血脂、吸烟、高血压等)、改善患者生活方式以及心血管病药物治疗,可减少乳腺癌放疗患者心血管疾病死亡率。
本研究建立在既往有关乳腺癌放疗与心血管疾病死亡率相关性的研究基础上,研究发现,乳腺癌基础风险高、接受左侧放疗、放疗体位为仰卧位的女性,发生心血管事件风险率最高;通过控制基础心血管疾病的危险因素、改善患者生活方式以及心血管病药物治疗,可减少乳腺癌放疗患者长期心血管疾病死亡率。
研究背景:
随着对乳腺癌认识的不断深入,以及治疗理念的转变与更新,乳腺癌的治疗进入了综合治疗时代,形成了乳腺癌局部治疗与全身治疗并重的治疗模式。主要包括手术、放疗、化疗、内分泌治疗、生物靶向治疗及中医药辅助治疗等多种手段。乳腺癌放疗是利用放射线破坏癌细胞的生长、繁殖,达到控制和消灭癌细胞的作用。由于目前科学条件所限,很难将放疗区域局限于癌组织,因此,乳腺癌的放射治疗难免会影响周边组织。
目前,既往研究证实,乳腺癌后放疗可增加患者急性冠脉事件、血栓栓塞事件、以及缺血性心肌病的患病率。并且,放疗暴露率越高,患者心血管疾病的发生率越高。除此以外,由于心脏位于左侧,因此左侧接受放疗的患者,其心脏受影响更大。
这些研究结果提示,接受放疗的乳腺癌患者,需警惕心血管疾病的发生。尤其是对于基础心血管疾病风险较高以及心脏与胸壁距离较近的的患者更应引起重视。除此以外,对于这些患者,通过控制基础心血管疾病的危险因素、改善患者生活方式以及心血管病药物治疗,可减少乳腺癌放疗患者长期心血管疾病死亡率。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








学习了,谢谢作者分享!
60
#DIC#
29
#CIN#
34
#eRNA#
36
#死亡风险#
31
#血管疾病#
23
#Medicine#
19
#Med#
20