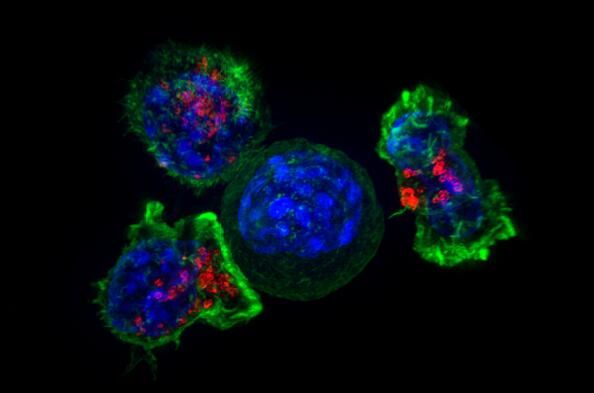
EMA授予AZ和MSD公司MEK抑制剂孤儿药资格用于治疗1型神经纤维瘤
2018-08-03 MedSci MedSci原创
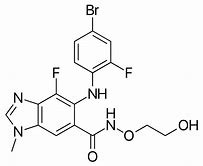
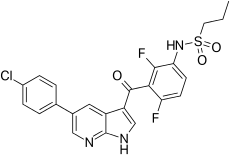
EMA授予阿斯利康(AZ)和默沙东(MSD)共同开发的MEK 1/2抑制剂司美替尼(Selumetinib)孤儿药资格,用于治疗1型神经纤维瘤病(NF1)。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#AZ#
41
#MEK#
32
#抑制剂#
39
谢谢了,学习
77
谢谢了。学习
69
谢谢了,学习
76
#EMA#
29
#1型神经纤维瘤#
38
#神经纤维#
27
#MEK抑制剂#
34