Autoimmun Rev:静脉注射免疫球蛋白可有效改善系统性硬化症的皮肤受累情况
2022-01-11 MedSci原创 MedSci原创
静脉注射免疫球蛋白(IVIG)是系统性硬化症SSc的一种新治疗方法。据推测,IVIG具有免疫调节和抗纤维化的活性。IVIG通常具有良好的耐受性,副作用很少。
静脉注射免疫球蛋白(IVIG)是系统性硬化症SSc的一种新治疗方法。据推测,IVIG具有免疫调节和抗纤维化的活性。IVIG通常具有良好的耐受性,副作用很少。本研究旨在验证IVIG对SSc皮肤受累的有效性。此外,还对迄今为止在SSc中使用静脉免疫球蛋白(IVIG)的结果进行了系统的文献回顾(SLR)。
研究人员评估了24名难治性弥漫性SSc皮肤受累患者(21名女性,3名男性)的数据(平均年龄为52.13岁)。2002年至2019年期间开始输注IVIG,剂量为2g/Kg体重,连续4天/月。治疗前用改良的Rodnan皮肤评分(mRSS)评估皮肤受累情况,然后在6和12个月后再次评估。为了进行SLR,从1990年到2020年在PubMed、Medline、Embase和Web of Science数据库中进行了搜索(关键词:IVIG、系统性硬化症)。
结果,研究最终确定了17篇论文(治疗患者总数为183人)。根据每项研究中考虑的器官受累情况,以及规定的剂量(大剂量或小剂量)和治疗方案,对这些研究进行了分类。在选定的论文中,主要涉及的器官是皮肤、胃肠道、关节和心血管系统。只有在一个病例中,血浆置换与IVIG有关。所有的论文都报道了皮肤受累的明显减少,但是由于缺乏对照病例或涉及的病人数量少,多数研究的证据质量有限。从现实生活中的经验来看,在6个月的随访中,mRSS明显减少(平均值为-6.61±5.2,P<0.001),并在12个月后保持稳定(-11.45±9.63,P<0.002)。
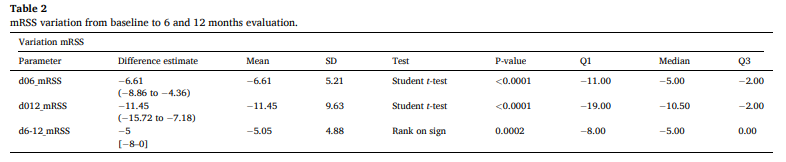
综上所述,这项SLR和回顾性研究的数据表明,IVIG可以改善皮肤受累情况,减少mRSS,特别是在那些对其他标准护理疗法难治的患者中,或是对合并肌炎患者的一种治疗选择。
原始出处:
Elana Agostini, et al., Intravenous immunoglobulins reduce skin thickness in systemic sclerosis: evidence from Systematic Literature Review and from real life experience. Autoimmun Rev. 2021 Dec;20(12):102981. doi: 10.1016/j.autrev.2021.102981.

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#硬化症#
40
#系统性#
27
#静脉#
40
#球蛋白#
38
#免疫球蛋白#
46
#静脉注射#
52
#系统性硬化#
32