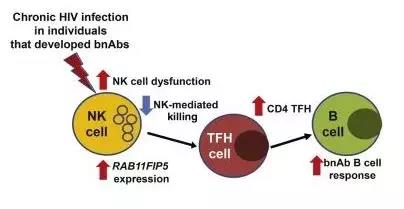
Cell:人体生产保护性HIV抗体的VIP绿道
2018-09-30 小通 生物通
只有大约一半的HIV感染者可以产生广泛的中和抗体(bnAbs),通常在病毒反复突变并插入宿主细胞基因组很久以后才得以生成,因时机过晚而失去效果。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#CEL#
34
#VIP#
55
#Cell#
45
#HIV抗体#
39
#生产#
42