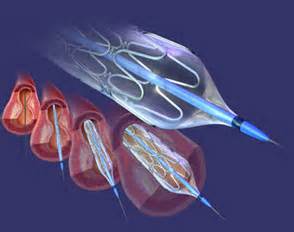
Lancet:治疗冠状动脉狭窄,选择依维莫司生物可吸收支架还是金属支架?
2016-10-31 MedSci MedSci原创
依维莫司洗脱生物可吸收血管支架和依维莫司洗脱支架效果的随机比较还没有可用的中期数据。
依维莫司洗脱生物可吸收血管支架和依维莫司洗脱支架效果随机比较还没有可用的中期数据。该研究旨在证明生物可吸收支架的两个机械性质:由于支架血管的血管舒缩恢复,腔内尺寸的增加。
ABSORB II试验是一项前瞻性,随机,单盲,平行两组,多中心临床试验。研究人员招募了年龄在18-85岁的符合条件的患者,这些患者患有心肌缺血,并且在不同心外膜血管中有一个或两个新生的天然损伤。研究人员随机分配患者(2:1)接受依维莫司洗脱生物可吸收支架(Absorb; Abbott Vascular,Santa Clara,CA,USA)治疗或用依维莫司洗脱金属支架(Xience; Abbott Vascular,Santa Clara, CA,USA)治疗。随机分组由糖尿病状态和计划的靶病变数量进行分层。在随访3年时,主要终点是Absorb生物可吸收支架与Xience金属支架在施用冠状内硝酸盐后血管造影血管反应性的优势。共同主要终点是血管造影晚期腔内损失的非劣效性。
在2011年11月28日至2013年6月4日期间,研究人员招募了501例患者,随机分为Absorb组(335例,364例病变)或Xience组(166例,182例病变)。在3年时两组间的血管舒缩反应性无统计学差异(Absorb组0,047mm [SD 0.109] vs Xience组0.056mm [0.117];Pnon-inferiority=0.49),而Absorb组比Xience组晚期腔内损失更大(0.37mm [0.45] vs 0.25mm [0.25]; Pnon-inferiority =0.78)。研究人员通过血管内超声评估最小管腔面积(4.32mm2 [SD 1.48] vs 5.38mm2 [1.51]; p <0.0001)证实了腔尺寸的这种差异。以患者为导向的复合终点,西雅图心绞痛问卷评分和运动测试的次要终点在两组中没有统计学差异。然而,Absorb组和Xience组之间的以设备为导向的复合终点差异显著(10% vs 5%,风险比2.17 [95%CI 1.01-4.70];对数秩检验P=0.0425),这主要是由靶血管心肌梗死(6% vs 1%; P=0.0108)引起的,包括围手术期心肌梗死(4% vs 1%; P=0.16)。
该试验没有满足其关于Absorb生物可吸收支架与金属支架相比,血管舒缩反应性和晚期腔内损失非劣效性的共同主要终点,与Absorb生物可吸收支架相比,金属支架可显著降低后期管腔损失。在Absorb组中,由于靶血管心肌梗死(包括围手术期心肌梗死)导致的以装置为导向的复合终点发生率更高。在3年时,对于以患者为导向的复合终点,心绞痛状态和运动测试在两个装置之间没有统计学差异。未来的研究应该调查精确血管内成像在设备尺寸和优化支架植入方面的临床影响。生物可吸收支架植入后长期双重抗血小板治疗的益处和需要也可能成为未来临床研究的主题。
原始出处:
Patrick W Serruys,Bernard Chevalier,Yohei Sotomi,et al.Comparison of an everolimus-eluting bioresorbable scaffold with an everolimus-eluting metallic stent for the treatment of coronary artery stenosis (ABSORB II),Lancet,2016.10.31
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Lancet#
37
#金属支架#
27
#生物可吸收#
33
#冠状动脉狭窄#
46
#可吸收#
46
#动脉狭窄#
23