Int J Cancer:尿前列腺素E2代谢产物与胰腺癌风险的前瞻性研究
2017-08-31 MedSci MedSci原创
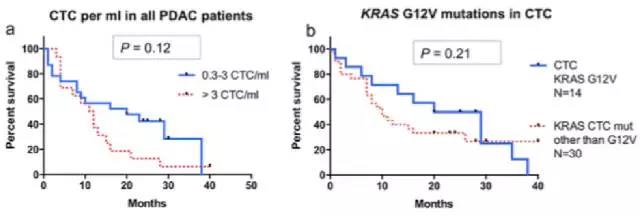
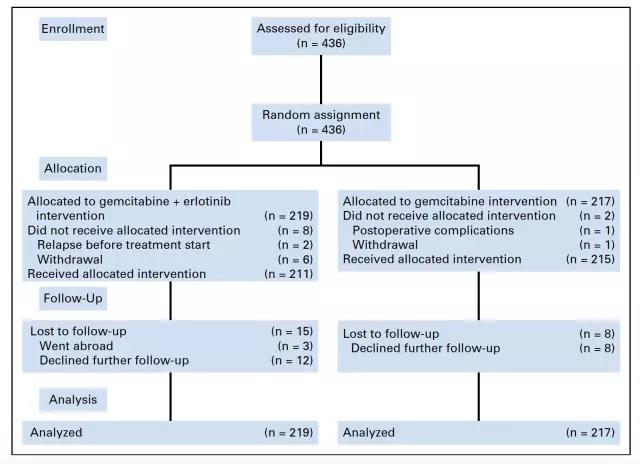
环氧合酶2(COX-2)通路在许多胰腺癌细胞中的表达是上升的,前列腺素E2(PGE2)作为COX-2催化花生四烯酸而产生的中间产物,在多种肿瘤中表达显著增加,且与肿瘤的发展相关。因此,有人认为COX-2上调的致癌作用主要是通过前列腺素E2(PGE2)的生产过剩造成的。来自美国的研究小组通过评估尿PGE2代谢物(PGE-M,体内PGE2生产过剩的一种生物标志物)和胰腺癌风险之间的相关性来验证这一假说
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#前瞻性#
46
#癌风险#
39
#前列腺素#
45
学习一下很不错
59
#前瞻性研究#
43
未来的发展前景广阔
63
好文.值得点赞!认真学习了.把经验应用于实践.为患者解除病痛.
69
#代谢产物#
55
#前列腺素E2#
41
谢谢了.学习
60