Neurology:颅内动脉狭窄增加MCI进展至AD的风险
2014-04-22 米怀 dxy
为了评估颅内动脉狭窄对轻度认知功能障碍患者进展至AD的影响,来自中国第三军医大学Jie Zhu博士的研究表明:颅内动脉狭窄增加轻度认知功能障碍患者进展至AD的风险。【原文下载】该研究为前瞻性研究,共连续入组423个轻度认知功能障碍病人,排除痴呆、卒中等病人。每年评估一次临床和神经心理学测试,共随访四年;记录随访期内AD性痴呆的发病率。颅内动脉狭窄根据颈部CTA测定,共分三个级别;MCI的评定主要根
为了评估颅内动脉狭窄对轻度认知功能障碍患者进展至AD的影响,来自中国第三军医大学Jie Zhu博士的研究表明:颅内动脉狭窄增加轻度认知功能障碍患者进展至AD的风险。【原文下载】
该研究为前瞻性研究,共连续入组423个轻度认知功能障碍病人,排除痴呆、卒中等病人。每年评估一次临床和神经心理学测试,共随访四年;记录随访期内AD性痴呆的发病率。
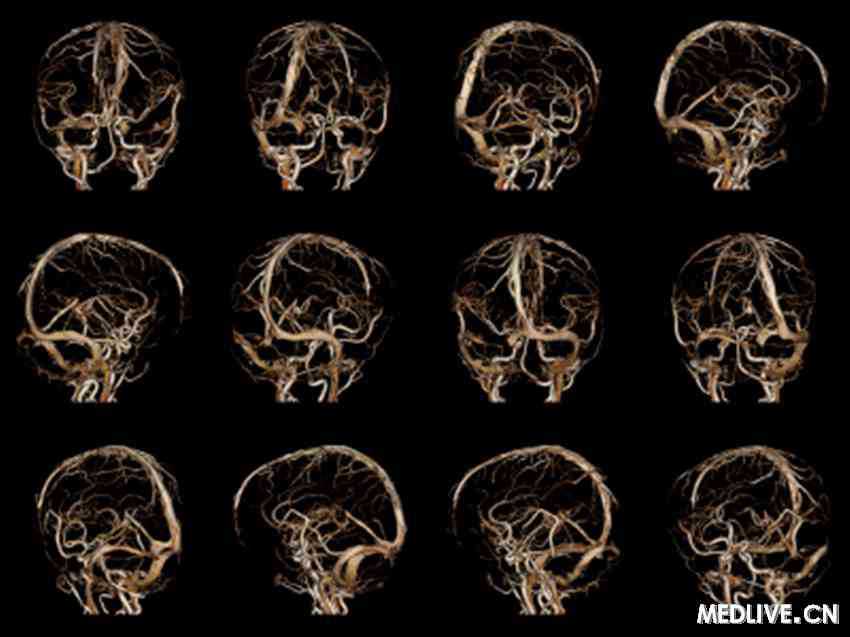
颅内动脉狭窄根据颈部CTA测定,共分三个级别;MCI的评定主要根据简易精神状态量表(MMSE)和日常生活能力量表(ADL:弥补简易精神状态量表不能反映执行功能的缺陷)。采用混合线性模型用来分析颅内动脉狭窄程度和MCI进展之间的关系;采用Cox比例风险模型分析颅内动脉狭窄和痴呆进展之间的关系。
截止到随访期终止,共116个参与者进展至AD性痴呆,仍保持在MCI状态的有223人。有中到重度颅内动脉狭窄的病人较无狭窄者认知功能下降更快,而且明显增加痴呆进展的风险,即使调整年龄、性别、教育、血管危险因素和临床沉默的MRI病灶(腔梗、脑白质病变)。
混合线性模型用来分析颅内动脉狭窄程度和MCI进展之间的关系,二级和三级颅内动脉狭窄患者在MMSE评分上下降更快,每年分别下降0.40和1.21,而1级的颅内动脉狭窄患者仅下降0.22;ADL评分结果也类似。
二者之间关系的可能机制为动脉粥样硬化不仅引起血管扭曲和缠绕,而且引起主要颅内血管的机械性闭塞;另外,大的颅内动脉粥样硬化性狭窄可能表明全身系统性动脉粥样硬化和广泛的微血管病变,引起微循环缺损,增加小血管阻力,降低血管反应性,最终导致脑灌注降低。而这些相互依存的血流动力学障碍累计效应可能在加速AD发病和进展中起重要作用。
这篇文章表明伴颅内动脉狭窄的MCI病人更易认知功能恶化和进展为AD性痴呆。鉴于目前针对AD特异性和有效性的治疗还不太可能实现,评估颅内动脉狭窄程度也许可以作为一个有效的临床工具去预计病人发展为AD的风险;而且,通过生活方式的调节以及应用抗动脉粥样硬化药的应用,也许可以阻止AD的发生或进展为AD。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#颅内动脉狭窄#
38
这个还是很有用的。
117
#Neurol#
36
#动脉狭窄#
36
#MCI#
55