Hypertension:瑞金医院朱鼎良等发现“血压晨峰”与无症状颅内动脉狭窄密切相关
2013-10-28 sunight dxy
研究要点:1.高血压患者颅内动脉狭窄的发生率较高;2.晨时的收缩压与高血压患者无症状颅内动脉狭窄相关。人体在一天内的不同时间段,血压会有所波动。不同时间段日间血压与脑血管损伤的关系尚不明确。此横断面研究共随机连续纳入757例高血压病患者,使用24小时动脉血压检测研究颅内动脉狭窄与收缩压间的关系。颅内颈动脉狭窄采用CT血管成像的方法进行检测,共发现127例(16.8%)颅内动脉狭窄患者,其中64例(
研究要点:
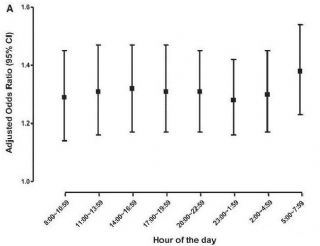
在调整心血管的危险因素及一天内其他时间的收缩压等因素后,这种不同仍然存在。多因素回归分析显示,一天内不同时间内持续3小时的收缩压增高与颅内动脉狭窄明显相关。然而,当采用单因素回归分析持续3小时平均收缩压与颅内动脉狭窄的关系时,只有晨时五点至八点的收缩压与颅内动脉狭窄相关。
总的说来,该研究显示除了传统的心血管因素外,晨时的收缩压与高血压患者无症状颅内动脉狭窄相关。该发现提出了晨时收缩压为脑血管病的重要危险因素,还需要后续研究对此进行验证。
人体血压存在昼夜节律性,通常夜间血压较清晨血压低。清晨觉醒后血压会迅速升高,出现血压晨峰现象。心脑血管疾病的发生也有明显的昼夜节律。有研究显示,血压晨峰与脑血管事件高发的时段一致,因此,血压晨峰与脑血管病可能密切相关。
原文出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#TENS#
34
#PE#
33
#颅内动脉狭窄#
36
#无症状#
43
#动脉狭窄#
33
#Hypertension#
37