Injury:弹性髓内针辅助复位经皮钢板内固定治疗锁骨中段粉碎骨折
2013-06-18 Injury dxy
近日有来自韩国的骨科医生将弹性髓内钉技术和经皮钢板内固定技术相结合成功治疗14例锁骨中段粉碎性骨折,术后未发现明显并发症,相关技术方法发表在injury杂志上。
按照传统观点,锁骨中段骨折通常采取保守治疗,但是鉴于锁骨中段粉碎性骨折保守治疗较多的术后并发症,如骨折不愈合,畸形愈合,锁骨缩短等,目前学界倾向于对这些患者采取更加积极的手术治疗。尽管切开复位内固定术是目前治疗锁骨骨折的金标准,但其术后并发症仍不少见,如骨折不愈合或感染等。为克服这些困难,有医生将弹性髓内钉技术应用在锁骨中段粉碎性骨折中,但该技术方法缺点在于固定效果不确切,术后存在内固定移位,缩短,断端重叠等可能性;经皮钢板内固定技术以其较好的骨折固定和愈合效果受到广大医生推崇,但因锁骨特殊的形态结构,经皮钢板内固定术中骨折复位和维持较为困难。近日有来自韩国的骨科医生将弹性髓内钉技术和经皮钢板内固定技术相结合成功治疗14例锁骨中段粉碎性骨折,术后未发现明显并发症,相关技术方法发表在injury杂志上。
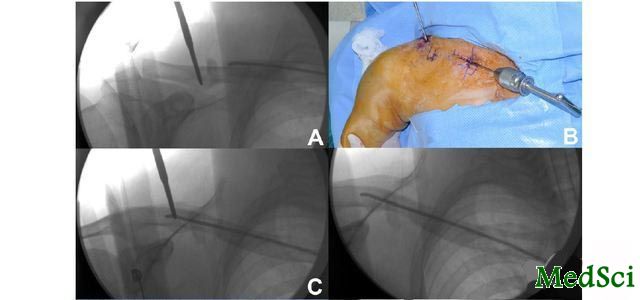
研究者回顾性分析了2009-2010年因锁骨中段粉碎性骨折住院治疗的患者。共15例患者符合研究纳入标准,所有患者均为锁骨B2.1或以上分型的骨折,其中14例患者获得术后至少12月随访,11例男性,3例女性,平均年龄42.9岁,相关人口统计学数据见表1.
表1:研究纳入患者的人口统计学数据
手术技术:
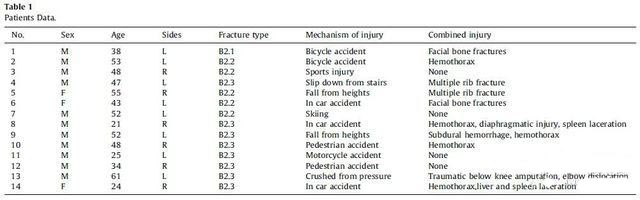
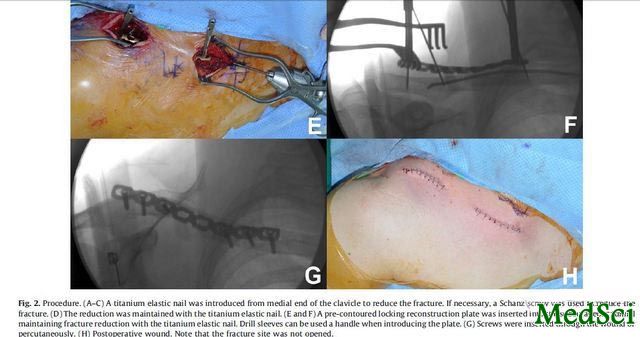
在麻醉达成前预备好需要的内固定材料。所需要的内固定材料为锁定或非锁定重建钢板,远近端钢板螺钉孔数至少有3枚可供固定。通过一个锁骨模型进行钢板的预弯以使钢板服帖。全麻后,患者仰卧位放置,患者肩关节垫高,以获得较好的手术术野。常规消毒铺巾。在距离锁骨内侧头2cm处做皮肤切口,在C臂机透视下使用2或2.5mm钛弹性髓内钉从锁骨髓腔穿入,进过骨折断端,维持骨折复位情况,若复位困难,可在骨折远端打入一枚4.0mm施氏针进行撬拨,协助骨折复位。而后在锁骨骨折近,远端锁骨表面皮肤开口2-3cm,使用器械沿锁骨行走区域在两开口间建立皮下隧道,经皮下隧道置入钢板而不暴露骨折端,确定钢板处于正确位置后使用两枚克氏针在近远端临时固定钢板以维持钢板和骨折复位位置,在近端及远端各攻入1-2枚螺钉固定钢板,后取出临时固定的弹性髓内钉,再经皮置入其余的皮质骨或锁定螺钉。术中无需断端植骨。如图1,2,3,4所示。
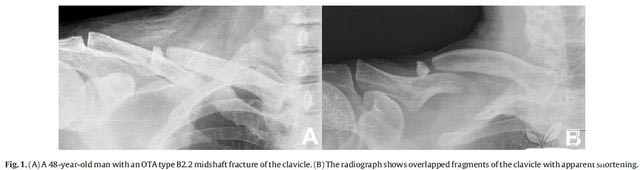
图1:a,48岁男性,OTA B2.2型锁骨中段骨折;b,影像学X片提示锁骨中段骨折端重叠,锁骨显著缩短
图2:手术过程:A-C:在距离锁骨内侧头2cm处做皮肤切口,在C臂机透视下使用2或2.5mm钛弹性髓内钉从锁骨髓腔穿入,进过骨折断端,维持骨折复位情况,若复位困难,可在骨折远端打入一枚4.0mm施氏针进行撬拨,协助骨折复位。D:弹性髓内钉维持骨折复位。E-F:经皮放置经过事先塑形的重建钢板,在钢板螺钉孔钻孔时使用钻套保护。G:经皮肤切口或皮肤钻入螺钉。H:术后皮肤切口,骨折端未切开。

图3:A-B,术后当时X片,3.5mm事先塑形后的锁骨重建板放置骨折锁骨表面。
图4:A-B:术后11周,骨折断端骨痂形成,桥接两骨折端,患侧和健侧锁骨长度差别细微。C,患者肩关节运动度良好。D,术后疤痕较小。
术后患肢悬吊,在无疼痛情况下可行上肢肩关节功能锻炼。术后复查X片,若出现骨折愈合征象,则可开始患肢负重。
术后6月及12月随访患者的肩关节Constant功能,DASH评分;术后1,2,3,6,12月影像学随访骨折愈合情况和术后并发症情况,通过健侧和患侧锁骨对比,评估骨折愈合,锁骨缩短等情况。
术后平均随访17.6月(15-31月),伤后到接受手术时间5.1天(1-15天),11例患者使用锁定重建板,3例使用普通重建板,平均手术透视时间109s,手术时间92min。
术后结果显示:
随访6月,肩关节Constant评分97分,平均DASH评分5.5分;12月时分别为99分,4.2分。所有患者术后肩关节活动良好,可以恢复到伤前水平;手术切口愈合良好。
影像学检查显示,术后平均愈合时间15.6周(11-18周),无患者出现骨折不愈合或延迟愈合。锁骨缩短比例0.4%(-1.5%-2.4%),无患者术后出现骨折部位钢板突出。
未发现患者出现术后并发症,如钢板断裂,感染,螺钉松动,再手术等。
研究者在讨论中认为,弹性髓内钉联合经皮钢板内固定技术具有以下技术优势:弹性髓内钉进行骨折复位时无需暴露骨折断端,可以最大限度的保证骨折断端血液供应,以利后期愈合;经皮钢板内固定技术在弹性髓内钉辅助复位下可以维持较好的骨折断端复位,同时避免弹性髓内钉固定不牢靠的缺点。两技术联合治疗锁骨中段粉碎性骨折术中骨折复位简便,术后骨折愈合率高,无明显切口感染,血管神经损伤等并发症,是一项值得推广的技术。
[编者按]这是一个非常实用的方法,这个方法在临床实践中有些地方也在做的,差别无非在于不是使用弹性髓内钉,而是以克氏针替代髓内复位。有个问题需要各位战友讨论一下:在近端有弹性髓内钉的情况下如何攻入钢板螺钉,非锁定板可以调整螺钉的进针方向,避开髓内钉;但锁定钢板是没办法调整螺钉角度的,如何在螺钉行走区域避免钻孔时和髓腔内的髓内钉撞针?请各位战友不吝赐教!

Percutaneous plating for comminuted midshaft fractures of the clavicle: a surgical technique to aid the reduction with nail assistance.
INTRODUCTION
Due to the complex anatomy of the clavicle, percutaneous plating with indirect reduction for comminuted midshaft fracture of the clavicle is challenging. The aim of this series was to report on a novel technique of nail-assisted percutaneous plating and to evaluate the radiographic and clinical outcomes in comminuted midshaft fractures of the clavicle.
MATERIALS AND METHODS
Between 2009 and 2010, with nail assistance for the reduction and its maintenance, percutaneous plating was performed in 14 patients with comminuted midshaft fracture of the clavicle. The mean follow-up period was 17.6 months (range, 15-31 months). A retrospective review of the clinical and radiologic results for these patients was conducted.
RESULTS
All fractures healed within a mean period of 15.6 weeks (range, 11-18 weeks) without loss of reduction. Regarding complications, there was no occurrence of implant failure or infection. All patients showed excellent shoulder function, with a mean Constant shoulder score of 99, and a mean Disabilities of the Arm, Shoulder and Hand (DASH) score of 4.2 (range, 0-22) at the latest follow-up. No significant difference in mean proportional length was observed between injured and uninjured clavicles, with a mean of 0.4% (range, -1.5% to 2.4%).
CONCLUSIONS
Minimally invasive percutaneous plating for comminuted midshaft fractures of the clavicle, combining the advantages of elastic intramedullary nailing and percutaneous plating, may be a good option.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Injury#
49
#髓内针#
51
#锁骨#
0
#内固定#
43