Nature:发现第一个致二尖瓣脱垂的基因突变
2015-08-12 佚名 生物谷
近日在线发表在Nature杂志上的一篇研究中,美国麻萨诸塞州总医院的一个国际合作研究确认了第一个引起二尖瓣脱垂(MVP)常见形式的‘突变基因——DCHS1突变。在三个受遗传性MVP影响的家庭中,每个人体内都发现了DCHS1突变。资深作者Susan A. Slaugenhaupt博士是麻州总医院研究所主任,并担任哈佛医学院的遗传学(神经学)教授。她表示:“这项工作提示了对调节瓣膜生长和发展的信号途
近日在线发表在Nature杂志上的一篇研究中,美国麻萨诸塞州总医院的一个国际合作研究确认了第一个引起二尖瓣脱垂(MVP)常见形式的‘突变基因——DCHS1突变。在三个受遗传性MVP影响的家庭中,每个人体内都发现了DCHS1突变。
资深作者Susan A. Slaugenhaupt博士是麻州总医院研究所主任,并担任哈佛医学院的遗传学(神经学)教授。她表示:“这项工作提示了对调节瓣膜生长和发展的信号途径的新见解,并提出了一个二尖瓣的长期结构完整性的基础。”另一位共同作者Robert Levine医学博士说:“这一发现可以让我们从遗传这种基因突变的人开始防止这种先天疾病。了解这种基因如何在瓣膜形成早期导致缺陷,使得我们了解如何防止这种情况的进展,以保持瓣膜和心脏健康,帮助患者避免发生并发症。”
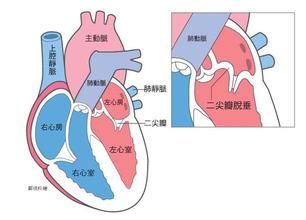
二尖瓣是控制心脏血液流动的四个瓣膜之一,位于左心房和左心室之间,处理从肺内返回的含氧血。该瓣膜由两个小叶组成,打开即让血液通过,关闭防止血液倒流。在MVP情况下,小叶加厚、变长和变软,瓣膜不能完全关闭,使得血液在返流过程倒流入心房。严重的MVP患者可能出现呼吸短促、心律不齐、心脏功能衰竭或心脏瓣膜的感染。MVP最常见的是在家族中出现。家族MVP的具体遗传原因在之前的研究中并没有被确定,而这次麻州总医院的研究团队第一次将家族性MVP的发生与一个位于11号染色体的遗传风险因子联系到一起。
在这个研究中,受MVP影响家庭成员进行详细的DNA分析,确定了DCHS1基因的两个罕见突变。斑马鱼的实验表明,DCHS1类似基因的失活会导致心脏对应二尖瓣的部位发展出现严重缺陷。但在引入人类DCHS1基因的正常拷贝后,缺陷能被显著预防。基于这些发现,研究小组寻求其他组织的合作,以确定是否其他MVP家庭成员也有相同的突变。通过分析后,研究人员确认了这个结果。随后,在细胞的进一步的实验表明,MVP相关这个突变显著降低了DCHS1蛋白,而DCHS1蛋白功能是帮助细胞们组织成形。在老鼠身上突变DCHS1基因的一个拷贝后,它的家庭成员也相应受到了影响。
这篇研究的结果显示,DCHS1基因在二尖瓣形成的过程中扮演重要角色,并且该突变导致二尖瓣出现类似于人类疾病的变化。这个发现是影响心脏发育的基因作用的第一个证据。研究人员表示他们会继续寻找其他导致MVP的基因突变。或许这将指向预防疾病的新目标。
原文出处:
Ronen Durst, Kimberly Sauls.et al.Mutations in DCHS1 cause mitral valve prolapse.
Nature.10 August 2015
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Nat#
29
我觉得这个发现的意义很重大
106
#二尖瓣脱垂#
33
#二尖瓣#
21