Br J Cancer:berzosertib+吉西他滨±顺铂联合治疗晚期实体瘤
2021-06-12 xiaozeng MedSci原创
包括铂类药物和吉西他滨(gemcitabine)在内的化疗药物会在癌细胞中诱导潜在的致命的DNA损伤反应(DDR),这是许多癌症标准疗法的一部分。
包括铂类药物和吉西他滨(gemcitabine)在内的化疗药物会在癌细胞中诱导潜在的致命的DNA损伤反应(DDR),这是许多癌症标准疗法的一部分。然而,化疗药物耐药性会导致患者较差的临床结果。与固有的和获得性耐药相关的一种机制是通过激活复杂DNA损伤修复机制。
DDR的顶端调节因子是ATM(共济失调毛细血管扩张突变激酶)和ATR(共济失调毛细血管扩张症和Rad3相关蛋白激酶),ATR主要对暴露的单链DNA有反应,这些单链DNA通常通过DNA损伤和复制应激所产生,而ATM则是对应着DNA双链断裂。
既往研究显示,抑制ATR是一种具有潜力的癌症治疗靶标,在这些癌症中,DNA损伤性化疗疗法已被用作标准疗法,但目前仍有待进一步的研究。
Berzosertib(M6620,VX-970)是一种高度有效的且选择性强的ATR抑制剂。该研究旨在评估耐药性/难治性晚期实体瘤患者的多次递增剂量的berzosertib+吉西他滨±顺铂联合治疗的疗效。
研究人员采用标准的3+3剂量递增治疗策略评估静脉注射berzosertib+吉西他滨±顺铂联合治疗的安全性、耐受性、药代动力学(PK)和初步疗效。治疗的起始剂量为berzosertib 18mg/m2,吉西他滨 875mg/m2和顺铂 60mg/m2。
相关研究设计图
结果显示,共52名患者接受了berzosertib+吉西他滨治疗,而另外八名患者接受了berzosertib+吉西他滨+顺铂的联合治疗。研究人员发现,接受berzosertib+吉西他滨治疗的四名患者共出现了七个剂量限制性毒性(DLT),而berzosertib+吉西他滨+顺铂治疗组则共出现了三个DLT。
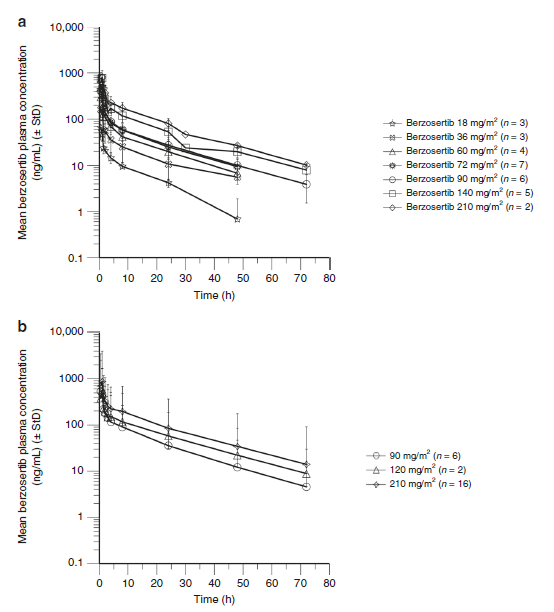
研究人员确定第2阶段推荐剂量(RP2D)为:berzosertib 210mg/m2(第2天和第9天)+吉西他滨 1000mg/m2(第1天和第8天);并没有确定berzosertib+吉西他滨+顺铂联合治疗的RP2D。进一步的研究显示,吉西他滨和顺铂均会不影响berzosertib的药代动力学。且大多数患者均取得了最佳部分缓解或疾病的稳定。
Berzosertib血浆浓度-时间曲线
总而言之,该研究结果揭示,晚期实体瘤患者对berzosertib+吉西他滨联合治疗的耐受性良好,且显示出了初步的疗效。
原始出处:
Middleton, M.R., Dean, E., Evans, T.R.J. et al. Phase 1 study of the ATR inhibitor berzosertib (formerly M6620, VX-970) combined with gemcitabine ± cisplatin in patients with advanced solid tumours. Br J Cancer (26 May 2021).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#铂#
39
#联合治疗#
34
#晚期实体瘤#
45
学习了
64
学习了!
81
吉西他滨加顺铂治疗
57