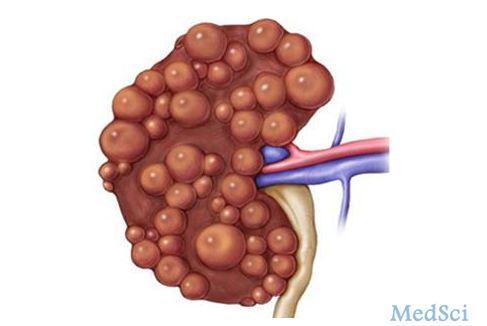
Lancet Oncol:多囊肾,警惕这些癌症
2016-09-08 Mechront 译 MedSci原创
本研究的目的旨在分析多囊肾患者固体固体癌症的风险。研究纳入了台湾1998年1月至2010年12月的≥20岁多囊肾患者,排除多囊肾患者、慢性肾脏病或终末期肾脏疾病患者。随访14年,主要终点为癌症诊断。研究纳入了4346例多囊肾患者和4346例非多囊肾对照组。多囊肾组和对照组中位随访时间分别为3·72年(IQR 1·25–7·31)和4·96年(2·29–8·38)。总癌症发病率在多囊肾病组更高(相比
本研究的目的旨在分析多囊肾患者固体固体癌症的风险。
研究纳入了台湾1998年1月至2010年12月的≥20岁多囊肾患者,排除多囊肾患者、慢性肾脏病或终末期肾脏疾病患者。随访14年,主要终点为癌症诊断。
研究纳入了4346例多囊肾患者和4346例非多囊肾对照组。多囊肾组和对照组中位随访时间分别为3·72年(IQR 1·25–7·31)和4·96年(2·29–8·38)。
总癌症发病率在多囊肾病组更高(相比对照组;20·1 [95% CI 18·3–21·9]/1000人年 vs 10·9 [10·1–11·8]/1000人年; cHR 1·77 [95% CI 1·52–2·07];aHR 1·83 [1·57–2·15](校正年龄、性别、就诊次数、合并症)。
对囊肾组的以下癌症风险显著高于对照组:肝癌(1·49 [95% CI 1·04–2·13]; p=0·030)、 结肠癌(1·63 [1·15–2·30]; p=0·006)、肾癌(2·45 [1·29–4·65]; p=0·006)。
这是首次调查非终末期肾脏疾病的多囊肾患者其癌症风险;这类患者的肝癌、结肠癌和肾癌显著更高,临床医务人员应清楚的认识到这一点,在诊疗过程中,意识到相应风险。
原始出处:
Tung-Min Yu.et al.Risk of cancer in patients with polycystic kidney disease: a propensity-score matched analysis of a nationwide, population-based cohort study.Lancet Oncol.Published Online: 19 August 2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Lancet#
38
#Oncol#
36
谢谢分享,很有用的信息
86
#多囊肾#
32
学习啦,谢谢分享
76
学习了谢谢。
58