NOACs对常规凝血试验的影响—案例分享ABC
2022-06-09 翁妙珊 南方医科大学附属潮州中心医院检验科 “检验医学”公众号
目前临床上正在使用的非维生素K拮抗口服抗凝药(NOACs)即新型口服抗凝药主要有两类:一类是凝血因子Xa直接抑制剂(艾多沙班、利伐沙班、阿哌沙班等);另一类是直接凝血酶抑制剂(达比加群酯)。
前 言
半个多世纪以来华法林是唯一的口服抗凝药物,近年来针对凝血过程中的关键环节成功研发了诸多作用于凝血瀑布过程中单一靶点,更加有效而安全的新型抗凝药物。具有治疗窗宽;固定剂量;无需监测;口服;疗效可预测;与食物、药物相互作用小、依从性好等优点。
目前临床上正在使用的非维生素K拮抗口服抗凝药(NOACs)即新型口服抗凝药主要有两类:一类是凝血因子Xa直接抑制剂(艾多沙班、利伐沙班、阿哌沙班等);另一类是直接凝血酶抑制剂(达比加群酯)。作为口服抗凝药的新成员,虽无需象华法林一样需要定期监测PT/INR,但它们对常规的凝血试验又有怎样的影响呢?
案例经过
案例A:
心血管内科患者男,66岁,首检凝血常规显示PT单独延长达17.2秒,余指标正常(图1)。查阅电子病例,患者因“反复心悸3个月”收治我院治疗。入院诊断:1.心房颤动、射频消融治疗术后;2.冠心病;3.高血压病,临床给予甲苯磺酸艾多沙班60mg/qd口服抗凝治疗。患者PT延长是因服用艾多沙班所致,该报告审核通过。
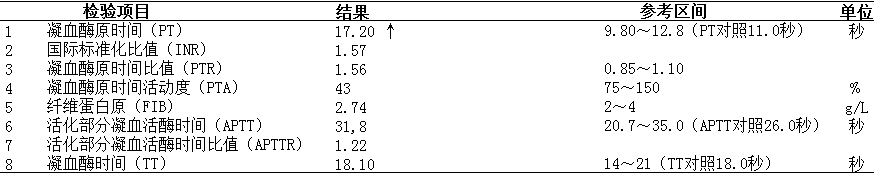
图1 案例A的凝血报告
案例B:
呼吸与危重症医学科患者女,59岁,首检凝血常规显示PT单独延长达25.4秒,余指标正常(图2)。与临床沟通,被告知该患者口服拜瑞妥抗凝治疗。查阅电子病例,患者因“反复胸闷、气促半年,加重1周”收治我院治疗,入院诊断:1.右肺癌伴多处转移;2.子宫内膜恶性肿瘤;3.左下肢深静脉血栓形成;4.冠心病。临床给予利伐沙班20mg/qd口服抗凝治疗,患者PT延长是因服用利伐沙班所致,该报告审核通过,并同步做好沟通记录。
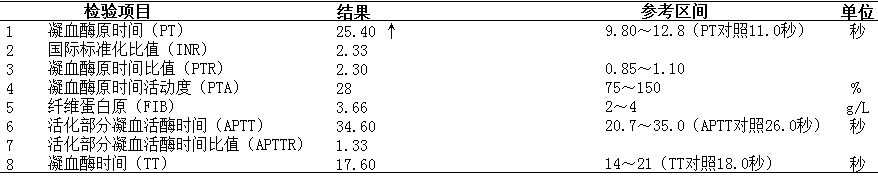
图2 案例B的凝血报告
案例C:
肿瘤科患者女,55岁,首检凝血常规显示PT12.9秒、APTT41.1秒、FIB5.06g/L、TT显着延长达166.1秒(图3)。与临床沟通,被告知该患者入院前一直规律口服达比加群酯110mg/bid进行抗凝治疗,查阅电子病例,患者因“右下肺腺癌靶向治疗1年余,腰背部疼痛4月余”收治我院治疗,入院诊断:1.晚期肺癌姑息治疗;2.右下肺腺癌并全身多处转移(脑、骨等)。患者的凝血异常是因服用达比加群所致,该报告审核通过,并同步做好沟通记录。
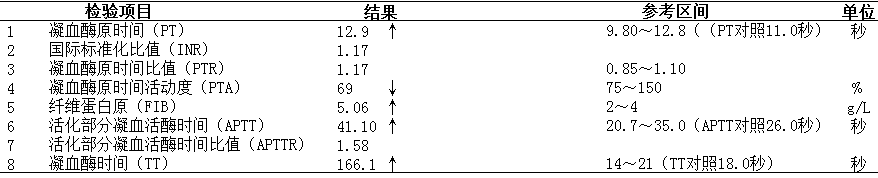
图3 案例C的凝血报告
案例分析
看到案例A和案例B的凝血结果,我们的检验科老师的第一反应是什么?可能猜想更多的是华法林抗凝吧,毕竟华法林是需要定期监测的一线抗凝药,但真相是:NOACs艾多沙班和利伐沙班。
艾多沙班和利伐沙班是直接FXa抑制剂,FXa是凝血共同途径上游的关键蛋白,主要功能是将凝血酶原转化为凝血酶并放大其生物学效应。直接FXa抑制剂能直接对抗游离和凝血酶原酶结合的FXa,影响凝血酶的生成和作用,从而达到抗凝的目的。
治疗剂量的艾多沙班和利伐沙班可影响PT结果,且大多数类型的PT试剂对两者的敏感性都高于阿哌沙班。APTT与两者的剂量相关性差,TT对两者不敏感。这两种NOACs对体外常规凝血试验的影响常表现为PT延长,APTT正常或轻度延长,而FIB、TT没有受到影响。
案例C是口服达比加群酯抗凝,达比加群酯是单靶点的因子Ⅱa(即凝血酶)抑制剂,在口服后通过非特异性酯酶转化为具有生物学活性的达比加群,不可逆地抑制血中游离及结合于纤维蛋白的凝血酶。
TT对血中达比加群有高度敏感性,故凝血试验常表现为TT的显着延长;APTT对血中达比加群中度敏感,但因为不同厂家APTT试剂的敏感性不同,因而APTT的延长程度会有所差别。PT对达比加群不敏感,常表现为正常或轻度延长。FIB通常不受影响,个别患者可能出现结果假性减低,其原因跟检测原理有关。
虽然FIB‐Clauss法采用的是足量的凝血酶,但如果患者服用的药物剂量较高或者FIB检测试剂中的凝血酶浓度较低,则会导致反应时试剂中的凝血酶含量不足,出现FIB‐C结果假性减低的情况。可通过稀释标本,点击仪器上的FIB‐CH模式(血浆加倍稀释,减低药物的干扰)重新检测FIB,或者补充FIB‐PT演算法结果并加以备注说明。
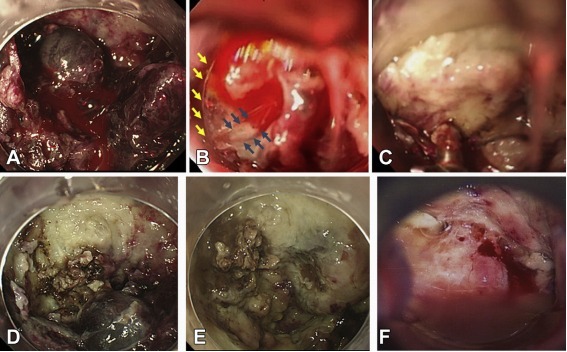
查阅相关文献资料,这三种NOACs对凝血常规的影响及基本特征总结如下(图4)。
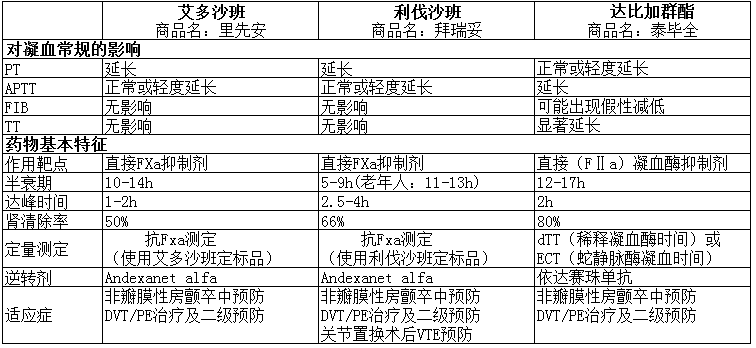
图4 三种NOACs对凝血常规的影响及基本特征
总结与心得
NOACs通常无需常规监测,直接FXa抑制剂的首选定量评估方法是药物校准的抗FXa发色底物法;药物校准的dTT和ECT可作为快速定量达比加群的合适方法,但这些试验目前临床实验室并未普遍开展。
那么,我们的常规凝血试验对药物的监测是否有所帮助呢?答案是肯定的。在更多的情况下,可通过常规凝血试验来迅速判断患者是否正在服用某种NOACs或药物过量,这对于药物过量的纠正和急诊手术的安全非常重要。例如,对于昏迷且急需急诊手术的患者需要明确是否在服用某种NOACs;对于肾功能突然恶化的患者则需要判断体内抗凝药物是否堆积。通常来说,当对某种NOACs敏感性低的凝血试验明显延长或者受到影响时,往往提示药物过量。
抗凝如同走钢丝,一边是血栓风险,另一边则是出血风险。抗凝药物更新迭代,随着NOACs在临床上的广泛应用,其安全问题也应该引起重视。检验人只有了解NOACs对常规凝血试验的影响,结合患者具体病史具体用药进行分析,才能更好的帮助临床去解读凝血报告,更好的为患者的健康保驾护航。
参考文献
[1] Tony.直接口服抗凝药对凝血检查的影响.血栓与止血实验室检查公众号.2021-10-12.
[2] 张鸿艳,任静,门剑龙.抗凝药物的实验室监测[J].中国心血管杂志,2019,24(6):565-570.
[3] 王学锋,吴竞生,胡豫,等.临床出血与血栓性疾病[M].第1版.北京:人民卫生出版社,2018:599-604.
[4] 赵晓静,门剑龙,任静.非维生素K拮抗口服抗凝药的实验室监测进展[J].临床检验杂志,2021, 39(5):321-326.
[5] 乔蕊.谈谈临床抗凝治疗对实验室监测的需求[J].临床检验杂志,2017, 35(12):892-894.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#ABC#
45
学习
33
#ACS#
41
#NOAC#
35
#NOACs#
41