新型股骨颈锁定钢板固定垂直剪切Pauwel C型股骨颈骨折的力学性能
2012-08-21 zhanghaisen 丁香园
年轻患者的股骨颈骨折通过切开复位内固定治疗可取的较佳的临床效果,骨折愈合率较高,而股骨头坏死机率相对较低。在股骨颈骨折手术的内固定选择上,目前以空心螺钉及动力加压钢板的应用最为广泛。髓内钉及其他一些锁定钢板等内固定物,临床也有应用,但研究报道较少。近日,美国Chattanooga医学中心的研究人员实施了一项生物力学研究,对一种新型股骨颈锁定钢板(femoral
年轻患者的股骨颈骨折通过切开复位内固定治疗可取的较佳的临床效果,骨折愈合率较高,而股骨头坏死机率相对较低。在股骨颈骨折手术的内固定选择上,目前以空心螺钉及动力加压钢板的应用最为广泛。髓内钉及其他一些锁定钢板等内固定物,临床也有应用,但研究报道较少。近日,美国Chattanooga医学中心的研究人员实施了一项生物力学研究,对一种新型股骨颈锁定钢板(femoral neck locking plate, FNLP)固定垂直剪切Pauwel C型股骨颈骨折的力学性能进行了实验测试,其研究结果发表在近期出版的Injury杂志上。
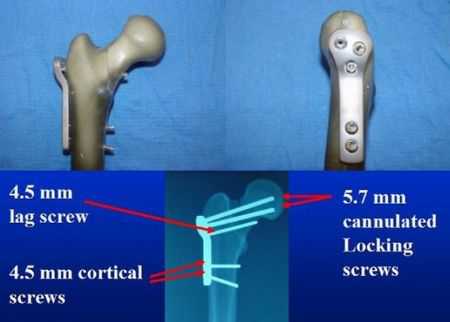
该研究进行了四种内固定物的力学实验。在研究中,首先创建40根股骨标本的垂直剪切Pauwel C型股骨颈骨折模型,并经标本分为4组,每组各采用一种内固定物对骨折进行固定,4种内固定物分别为平行空心螺钉3根(cancellous screws, CS);置入股骨颈头端的拉力空心螺钉2根和置入股骨距的拉力螺钉一根(XCS);5.7mm孔径新型锁定钢板(FNLP),钢板中2枚锁定螺钉置入股骨颈,1枚置入股骨距,另有2枚置入股骨干;2孔135°AMBI动力加压钢板及一枚防旋螺钉。骨折-内固定物结构创建完成后,测试4组标本固定结构的轴向(20000转)、旋转刚度的变化,并记录最大失效载荷。通过单因素方差分析(ANOVA)及Fisher-LSD法进行组间数据的比较。
图1.本研究中新型股骨颈骨折锁定钢板的正、侧位观:2枚5.7mm锁定空心螺钉置入股骨颈头端,1枚4.5mm皮质骨拉力螺钉置入股骨距,另外2枚双皮质螺钉经钢板置于股骨干。
图2.4种内固定方式的正、侧位X线透视图像。
图3.股骨近端力学测试装置的安装。
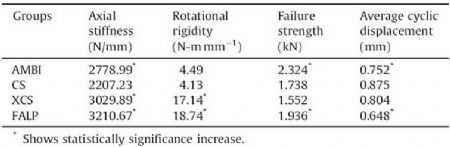
力学实验结果显示,AMBI, CS, XCS 以及FNLP 4组的轴向刚度分别为2779.0, 2207.2, 3029.9 和3210.7N-mmm−1 ;旋转刚度分别为4.5, 4.1, 17.1 和18.7N-mmm−1,平均循环位移分别为0.75, 0.88, 0.80 和0.65mm;最大失效载荷分别为2.3, 1.7, 1.6 和1.9kN。研究结果表明,FNLP固定结构的轴向刚度明显高于其他3种传统内固定结构。最后,作者认为,垂直剪切Pauwel C型股骨颈骨折采用PNLP固定的生物力学性能良好,但其应用于临床尚需进一步病例观察研究的证实。
表1.4组标本的轴向刚度,旋转刚度,失效强度以及平均循环位移测试结果(采用ANOVA进行数据比较)

图4.各组的轴向刚度测试结果对比(N-mmm−1)。
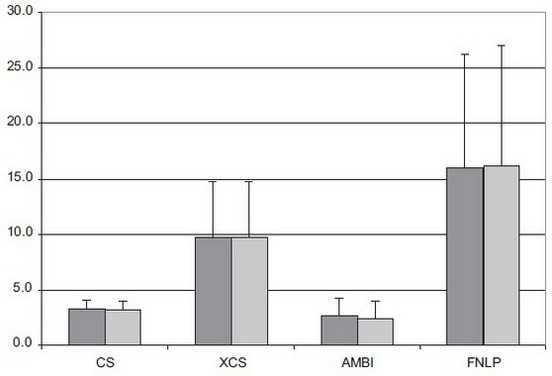
图5.各组的旋转刚度测试结果对比(N-mmm−1)。
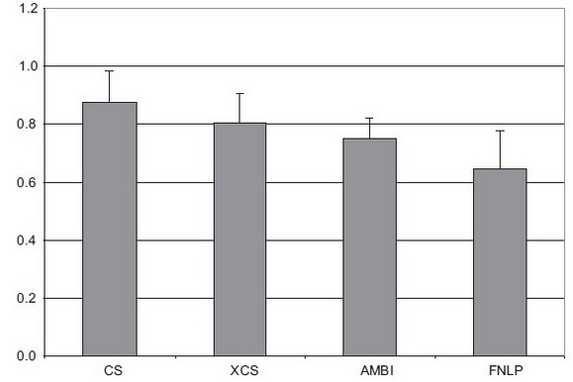
图6.各组的平均循环位移测试结果对比(mm)。
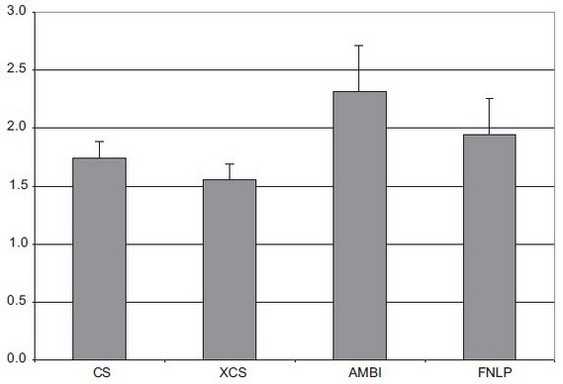
图7.各组的最大失效载荷测试结果对比(kN)。
Nowotarski PJ, Ervin B, Weatherby B, Pettit J, Goulet R, Norris B. Biomechanical analysis of a novel femoral neck locking plate for treatment of vertical shear Pauwel's type C femoral neck fractures. Injury. 2012 Jun;43(6):802-6. Epub 2011 Oct 21.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#股骨颈#
36
#股骨#
31
#股骨颈骨折#
27