European Radiology:直肠系膜脂肪的MRI放射组学特征与直肠癌患者的预后
2022-01-16 shaosai MedSci原创
MRI是直肠癌分期的标准成像方式,对于评估直肠癌局部进展(LARC)意义重大。
 MRI是直肠癌分期的标准成像方式,对于评估直肠癌局部进展(LARC)意义重大。在MRI上,直肠系膜,即直肠周围的内脏脂肪组织,由直肠系膜筋膜所包绕,因此显示清晰。一些有关直肠癌的研究表明,放射组学可以协助临床进行预后及治疗反应的预测,如对新辅助化疗的病理完全反应(pCR)、淋巴结状态或肝转移等。
MRI是直肠癌分期的标准成像方式,对于评估直肠癌局部进展(LARC)意义重大。在MRI上,直肠系膜,即直肠周围的内脏脂肪组织,由直肠系膜筋膜所包绕,因此显示清晰。一些有关直肠癌的研究表明,放射组学可以协助临床进行预后及治疗反应的预测,如对新辅助化疗的病理完全反应(pCR)、淋巴结状态或肝转移等。
越来越多的证据表明,肿瘤细胞对瘤内、瘤周、甚至远处的脂肪细胞之间的分子信号传递起着关键作用。这些分子相互作用可导致局部和全身的炎症标志物(脂肪因子)和血管生成因子(如VEGF或IGF-1)水平升高,促进肿瘤的生长和转移。因此,直肠肿瘤和直肠系膜脂肪之间的相互作用可导致脂肪细胞分子谱的变化,随后导致MRI上肉眼无法评估的细微变化,特别是在肿瘤进展的早期阶段尤为明显。迄今为止,只有少数研究在MRI上对瘤周组织进行放射组学评估,以预测临床结果、治疗反应或预后。
近日,发表在European Radiology杂志的一项研究利用MRI放射组学特征对直肠系膜脂肪进行分析,以进行局部进展期直肠癌患者临床预后及治疗效果的无创评估及预测。
本项回顾性研究纳入了2009年至2015年期间因直肠癌局部进展而接受新辅助化疗的患者。三位放射科医生在基线T2加权轴位MRI图像上独立分割直肠系膜脂肪。从分割的体积中提取放射组学特征,并使用CERR软件进行计算,采用自适应合成取样来对抗大类不平衡。结果变量包括病理完全反应(pCR)、局部复发、远处复发、临床T类(cT)、治疗后T类(ypT)和治疗后N类(ypN)。使用支持向量机和五倍交叉验证法选择最多八个最重要的特征进行模型开发,通过弹性网正则化来预测每个结果参数。计算了最终模型的诊断指标,包括敏感性、特异性、PPV、NPV、准确性和AUC。
该研究包括236名患者(54±12岁,135名男性)。每个临床结果的AUC、敏感性、特异性、PPV、NPV和准确性如下:对于pCR,0.89,78.0%,85.1%,52.5%,94.9%,83.9%;对于局部复发,0.79,68.3%,80.7%,46.7%,91.2%,78. 3%;远处复发,0.87,80.0%,88.4%,58.3%,95.6%,87.0%;CT,0.80,85.8%,56.5%,89.1%,49.1%,80.1%;ypN,0.74,65.0%,80.1%,52.7%,87.0%,76.3%;以及ypT,0.86,81.3%,84.2%,96.4%,46.4%,81.8%。
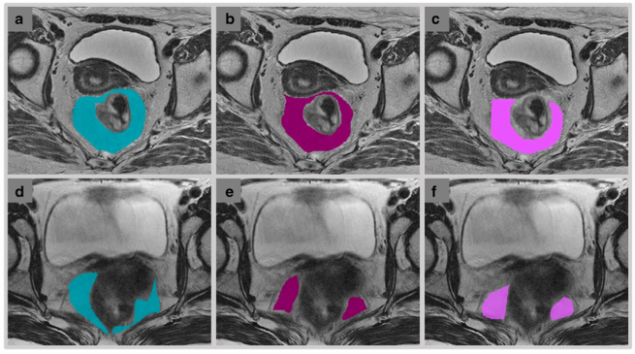
图 读者1(a)、读者2(b)和读者3(c)对一名66岁的女性直肠癌患者进行了直肠系膜脂肪的分割,Jaccard指数和Dice相似系数分别为0。 读者1(d)、读者2(e)和读者3(f)对一名48岁的女性直肠癌患者的直肠系膜脂肪进行了分割,Jaccard指数和Dice相似性系数分别为0.298和0.451。
据我们所知,本研究是迄今为止利用MRI放射组学对直肠系膜脂肪进行的最大研究。本研究数据表明,仅从直肠系膜脂肪得到的基于MRI放射组学的信息可预测直肠癌的各种临床预后及治疗反应,如pCR和局部及远处复发,为直肠系膜脂肪在直肠癌发病机制中不可或缺的作用增加了越来越多的证据。
原文出处:
Vetri Sudar Jayaprakasam,Viktoriya Paroder,Peter Gibbs.MRI radiomics features of mesorectal fat can predict response to neoadjuvant chemoradiation therapy and tumor recurrence in patients with locally advanced rectal cancer.DOI:10.1007/s00330-021-08144-w
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#PE#
30
学习
48
学习#学习#
50
#肠系膜#
44