NEJM:艾滋病患者接受ART后10年生存率能达七成
2016-02-01 MedSci MedSci原创
我们报道了一项关于艾滋病患者接受连续抗逆转录病毒治疗(ART)后10年生存率的队列研究,该研究来自海地太子港,纳入自2003至2004年间入院接受ART、且年龄大等于13岁的患者共910例,随访时间为10年;ART与随访期间护理均严格按照世界卫生组织(WHO)指南。该回顾性队列研究的有关细节已有报道,已获得有关机构审查委员会伦理学批准。死亡事件可从医疗记录中确定。转院患者资料在转院时审查。将随访终
一项来自海地太子港关于艾滋病患者接受连续抗逆转录病毒治疗(ART)后10年生存率的队列研究,该研究纳入自2003至2004年间入院接受ART、且年龄大等于13岁的患者共910例,随访时间为10年;ART与随访期间护理均严格按照世界卫生组织(WHO)指南。
该回顾性队列研究的有关细节已有报道(包括研究人群,以及5年的生存率,见附参考文献),已获得有关机构审查委员会伦理学批准。死亡事件可从医疗记录中确定。转院患者资料在转院时审查。将随访终点前超过180天无临床接触定义为失访。
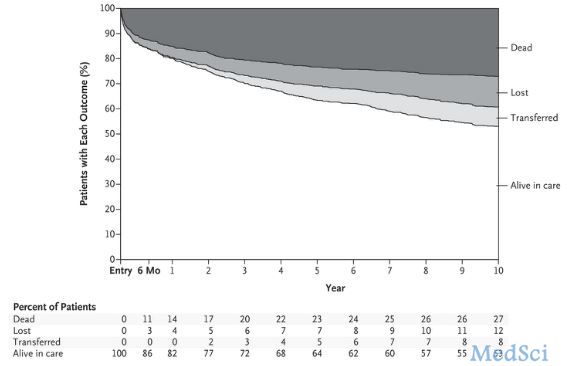
研究采用以下三种方法评估失访患者生存状态并估计10年生存率:Kaplan-Meier法审查失访时患者数据,逆概率加权法用于追踪数据,多重插补法可基于基线特征评估失访患者生存率。利用Cox模型确定10年生存相关特性。基线入组的910例患者中,女504例(55%),年龄中位数为39岁,CD4+T细胞计数中位数为131/mm3(四分位距为51-212)。近半数患者极度贫困,每日收入不足1美元。
通过Kaplan-Meier法、逆概率加权法( inverse-probability weighting)、多重插补法(multiple imputation )估算的10年生存率相似,分别为: 71%(95% CI,68~74)、63%(95% CI,59~67)、67%(95% CI,64~71)。
死亡患者中,42%死亡时间为接受治疗后6个月内;该期间患者死亡与男性、年龄大于50岁、体重在相应性别最低四分位数、合并WHO定义的III或IV期疾病、伴有活动性肺结核等因素相关(P<0.05)。6个月后死亡的危险因素包括:年龄大于 50岁、每日收入不足1美元、体重处于最低四分位数、治疗依从性处于最低四分位数等(P<0.05)。尽管2010年发生地震,该年死亡率与其它年份相比并无显著差异。
482例存活患者中,351例(73%)继续接受一线治疗,178例(37%)患有慢性非传染性疾病(其中心血管疾病109例、肺部疾病67例、糖尿病2例)。
在发展中国家,绝大部分患者接受ART时处于艾滋病晚期。该研究为首批关于发展中国家患者接受ART的大型队列研究之一,估算10年生存率为63%-71%,与美国接受ART的艾滋病早期患者生存率相似。研究结果表明,为资源匮乏的国家患者提供ART有赖于长期、可持续的国际合作。
原始出处:
Pierre S, Pape J, McNairy ML, Jannat-Khah D, Fitzgerald DW.10-Year Survival of Patients with AIDS Receiving Antiretroviral Therapy in Haiti. N Engl J Med. 2016 Jan 28;374(4):397-8.
ART治疗
鸡尾酒疗法,原指“高效抗逆转录病毒治疗”(HAART),由美籍华裔科学家何大一于1996年提出,是通过三种或三种以上的抗病毒药物联合使用来治疗艾滋病。该疗法的应用可以减少单一用药产生的抗药性,最大限度地抑制病毒的复制,使被破坏的机体免疫功能部分甚至全部恢复,从而延缓病程进展,延长患者生命,提高生活质量。该疗法把蛋白酶抑制剂与多种抗病毒的药物混合使用,从而使艾滋病得到有效的控制。
越来越多的科学家相信,混合药物疗法是对付艾滋病的最有效治疗方法,既可以阻止艾滋病病毒繁殖,又可以防止体内产生抗药性的病毒。近年来在其他疾病上,也有人将类似的联合用药疗法称为相对应的“鸡尾酒疗法”。
MedSci提示:
Kaplan-Meier法审查失访时患者数据,逆概率加权法用于追踪数据,多重插补法可基于基线特征评估失访患者生存率,这三种统计策略都进行了应用,也是常见的三种方法,你懂了吗?如果不了解这些,可以向MedSci提供相关服务哦
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#艾滋病患者#
32
有些哪
90
#生存率#
21
#ART#
29
希望有新的突跛
110
希望能有进一步进展
110
抗艾!
145
加油必胜
95