Lancet Neurol:颈动脉夹层抗血小板治疗与抗凝治疗的比较(CADISS试验)
2015-02-18 李志行 译 MedSci原创
颈外动脉和椎动脉夹层是引起中风的一个重要原因,尤其是对年轻人而言。在一些观测研究中,它与复发性脑卒中的高风险相关联。抗血小板药物和抗凝药物都被用来降低发生卒中的风险,但无法得知是否一种治疗策略要比另一种更为有效。我们对比了它们对卒中研究的颈动脉夹层(CADISS)的疗效,另外旨在确定复发性脑中风的真正风险。研究方法:我们在有专门的卒中或神经学服务的医院进行了本次随机试验(英国39所,澳大利亚7所)
颈外动脉和椎动脉夹层是引起中风的一个重要原因,尤其是对年轻人而言。在一些观测研究中,它与复发性脑卒中的高风险相关联。抗血小板药物和抗凝药物都被用来降低发生卒中的风险,但无法得知是否一种治疗策略要比另一种更为有效。我们对比了它们对卒中研究的颈动脉夹层(CADISS)的疗效,另外旨在确定复发性脑中风的真正风险。
研究方法:
我们在有专门的卒中或神经学服务的医院进行了本次随机试验(英国39所,澳大利亚7所)。我们将在过去7天内颈外动脉和椎动脉夹层症状发作的患者计入其中。通过自动语音随机化服务,患者被随机分配(1:1)接受3个月的抗血小板药物或抗凝药物(特定治疗由当地临床医生决定)。对于分配情况,患者和临床医师并不处于盲态,但是由研究者评估终点。主要终点是在意向性治疗人群中发生同侧中风或死亡。试验在EUDract (2006-002827-18) 和 ISRN (CTN44555237)进行了登记。
研究结果:
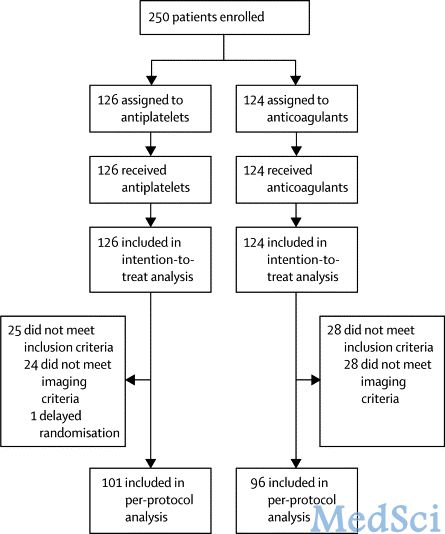
我们登记了250名参与者(118名颈动脉,132名椎动脉)。随机化的平均时间为3·65天(SD 1·91)。主要症状为卒中或短暂性脑缺血发作(n=224)和局部症状(头痛、颈痛或霍纳氏综合征;n=26)。126名参与者被分配给了抗血小板治疗,124名被分配给抗凝治疗。总的来说,250名患者中有4名(2%)卒中复发(都为同侧性)。126名患者中有3名(2%)发生了卒中或死亡,124名患者中有1名(1%)([OR] 0·335, 95% CI 0·006–4·233; p=0·63)。在抗凝组中没有死亡,但有一例大出血(蛛网膜下腔出血)。中心成像没能证实52名患者的夹层。预先计划的符合方案数据分析将抗血小板组101名患者中的3名(3%)和抗凝组96名患者中的1名(1%)中显示出卒中或死亡的患者排除在外(OR 0·346, 95% CI 0·006–4·390; p=0·66)。

3个月时主要研究结果
我们没有发现抗血小板和抗凝药物在预防有症状的颈动脉和椎动脉夹层患者发生卒中和死亡的疗效方面的区别,但是卒中在两组中都罕见,比一些观测研究中报道的要少得多。在很多情况下,夹层的诊断没有在观察后得到证实,显示出影像学标准并不总是正确地运用在日常临床实践中。
The CADISS trial investigators
Antiplatelet treatment compared with anticoagulation treatment for cervical artery dissection (CADISS):a randomised trial
Lancet Neurol 2015 Published Online February 12, 2015 http://dx.doi.org/10.1016/ S1474-4422(15)70018-9
本文是MedSci原创编译整理,转载需要事先获得授权!转载需要附来源及MedSci 原始链接。谢谢!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Neurol#
0
#颈动脉#
45
#Lancet#
30
#颈动脉夹层#
39
#Dis#
29
不错的文章,学习了
88
国外阴性文章真普遍
106
#动脉夹层#
26