European Radiology:IPMN的哪些影像学特征能够提高对恶性肿瘤的预测?
2022-07-21 shaosai MedSci原创
IPMN具有多种的不同生物学行为,从低级别的发育不良(LGD)到高级别的发育不良及浸润性癌(HGD/INV)。因
胰腺导管内乳头状粘液瘤(IPMN)是一种胰腺囊性肿瘤(PCN),经常在因其他原因进行的横断面成像(即CT和/或MRI)中偶然发现。IPMN具有多种的不同生物学行为,从低级别的发育不良(LGD)到高级别的发育不良及浸润性癌(HGD/INV)。因此,有必要对IPMN进行长期监测以及手术治疗以预防胰腺癌(PC)的发生。
根据目前的指南,有几个特征与IPMN患者的恶性肿瘤风险相关,其中包括囊肿大小。然而,囊肿直径仍然是一个有争议的问题,即使较小的囊肿也可并发HGD/INV。因此,目前还不清楚最大的囊肿直径是否能够为风险分层提供足够的信息。
由于IPMNs形态不规则,最大直径可能不能完全代表IPMNs的整个内表面,因此体积测定有助于对有恶性风险的IPMNs进行分层。此外,目前的指南建议根据其他特征以决定手术,包括主胰管(MPD)扩张、CA19-9血清水平升高、壁结节(MN)的存在以及监测期间囊性肿瘤的大小进展。。
近日,发表在European Radiology杂志的一项研究评估了在排除实性肿块形成的PC后,体积、形态和所有其他公认的RC特征在BD型和混合型IPMN患者恶性程度预测中的作用,为临床制定IPMN的最佳诊治流程及个性化治疗方案提供了参考。
本研究对106名经组织病理学诊断为BD型和混合型IPMN(无实体肿块)且术前有MRI的患者(2008-2019)进行了回顾性研究。收集标准的影像学和临床特征,并在T2加权图像上计算新的影像学特征囊肿体积和伸长值[EV=1-(宽度/长度)]。进行了Logistic回归分析。统计学意义设定为双尾,P < 0.05。
体积(OR=1.01,95%CI:0.99-1.02,P=0.12)和EV(OR=0.38,95%CI:0.02-5.93,P=0.49)都与恶性肿瘤无关。增强的壁结节(MN)、主胰管(MPD)≥5毫米、CA19-9血清水平升高(>37μmol/L)与恶性肿瘤有关(MN OR: 4.32, 95% CI: 1.18-15.76, p = 0.02; MPD ≥ 5 mm OR: 4.2, 95% CI: 1.34-13.1, p = 0.01; CA19-9 OR: 6.72; 95% CI: 1.89 - 23.89, p = 0.003)。
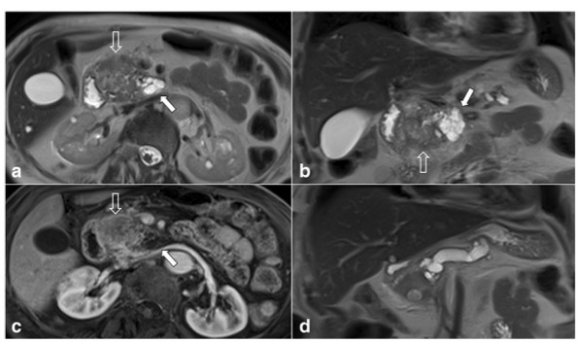
图 一位80岁患者的胰腺MRI图像。轴向(a)和冠状(b)T2加权图像显示一个位于胰腺头部的实性肿块状的胰腺癌(PC)(开放箭头),起源于邻近的IPMN(白色箭头)。胰腺癌在胰腺动脉期的T1-w轴位图像中呈均匀的低密度(c)。PC导致主胰管(MPD)狭窄,在冠状T2加权图像上显示上断扩张(d)。该患者被排除在我们的队列之外,因为继发于实性肿块的MPD扩张可能会导致高估 "MPD扩张 "这一发现的阳性结果
本研究表明,BD-IPMN的体积测量和其他新的影像学特征都不能实现对恶性肿瘤的预测。 MPD扩张、增强的MN和CA 19-9的血清水平异常升高有与较高的恶性肿瘤风险有关。
原文出处:
Raffaella M Pozzi Mucelli,Carlos Fernández Moro,Marco Del Chiaro,et al.Branch-duct intraductal papillary mucinous neoplasm (IPMN): Are cyst volumetry and other novel imaging features able to improve malignancy prediction compared to well-established resection criteria?DOI:10.1007/s00330-022-08650-5.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#PMN#
37
#PE#
43
#IPMN#
35
认真学习~~
40