Sci Rep:在肌肉侵入性膀胱癌中,膀胱部分切除术后的肿瘤结果、生活质量结果和并发症结果研究
2018-06-11 AlexYang MedSci原创
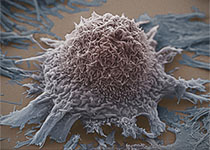
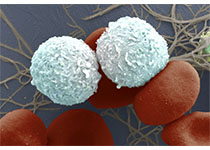
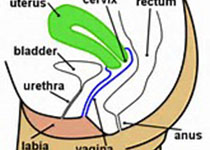
最近,有研究人员为了评估患有肌肉侵入性膀胱癌(MIBC)患者经历膀胱部分切除术(PC)后的肿瘤结果、相关的并发症和术后健康相关的生活质量(HR-QoL),他们进行了相关的研究,研究包括了27名经历了cT2 MIBC开放PC手术的患者。研究人员利用一个简单的Cox's比例风险回归模型来评估一些潜在的预后因素与生存的关系,利用EORTC QLQ-C30调查问卷3.0版本评估了术后HR-QoL。研究发现
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#并发#
38
#切除术#
25
#侵入性#
30
学习一下谢谢
62
学习一下谢谢
49
学习了
49