Science signaling:胰腺癌转移新套路——借力神经转移
2015-08-14 佚名 生物谷
近日,来自美国约翰霍普金斯Kimmel癌症中心的科学家在胰腺癌细胞中发现一种新的分子关系能够帮助解释胰腺癌转移的原因。美国每年有大约50,000人罹患胰腺癌,并且诊断后的5年生存率只有5%,而这一研究发现的促癌转移关键分子可能为胰腺癌治疗提供新的靶点。Annexin A2是一种参与多种癌症并导致病人生存率低下的蛋白分子。在这项发表在国际学术期刊science signaling的研究中,研究人员发
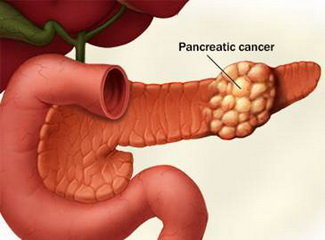
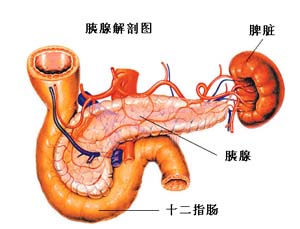
近日,来自美国约翰霍普金斯Kimmel癌症中心的科学家在胰腺癌细胞中发现一种新的分子关系能够帮助解释胰腺癌转移的原因。美国每年有大约50,000人罹患胰腺癌,并且诊断后的5年生存率只有5%,而这一研究发现的促癌转移关键分子可能为胰腺癌治疗提供新的靶点。
Annexin A2是一种参与多种癌症并导致病人生存率低下的蛋白分子。在这项发表在国际学术期刊science signaling的研究中,研究人员发现annexin A2能够引导一种叫做Sema3D的蛋白"逃逸"出胰腺癌细胞,一旦离开细胞,Sema3D能够与另外一种分子联结在一起助力癌细胞转移。
之前研究表明在神经细胞生长发育过程中,Sema3D能够引导神经细胞的轴突进行伸展,但人们对于Sema3D与胰腺癌转移之间存在何种关联了解较少。
研究人员利用胰腺癌小鼠模型进行了研究,他们发现在缺少annexin A2的小鼠体内,胰腺癌细胞分泌的Sema3D下降了70倍。而在进行的另外一项实验中,23只缺失annexin A2的胰腺癌模型小鼠均未发生可见的转移瘤,而可产生annexin A2的17只小鼠中有16只在肝脏,肺或腹腔内出现了转移瘤。
研究人员还对胰腺导管腺癌病人的组织进行了分析,同样发现Sema3D在组织内的丰度与转移性胰腺癌进展之间存在显著关联。同时,研究人员还指出,Sema3D似乎还与手术切除胰腺肿瘤的病人出现胰腺癌复发有关。
领导该项研究的Lei Zheng博士及其同事指出,他们还不清楚Sema3D究竟如何促进胰腺癌转移,但根据之前关于Sema3D功能的报道,他们认为Sema3D可能通过帮助癌细胞包绕和追踪神经远离主体瘤实现癌细胞的转移。
原文出处:
K. Foley, A. A. Rucki, Q. et al.Semaphorin 3D autocrine signaling mediates the metastatic role of annexin A2 in pancreatic cancer.Science Signaling.2015
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Sign#
21
#Signal#
36
#signaling#
26
应该关注一下这方面的进展
137
#SCIE#
22
#癌转移#
21