Cancer Cell:趋化因子可能是T细胞进入肿瘤细胞的关键
2019-06-27 北京义翘神州 生物通
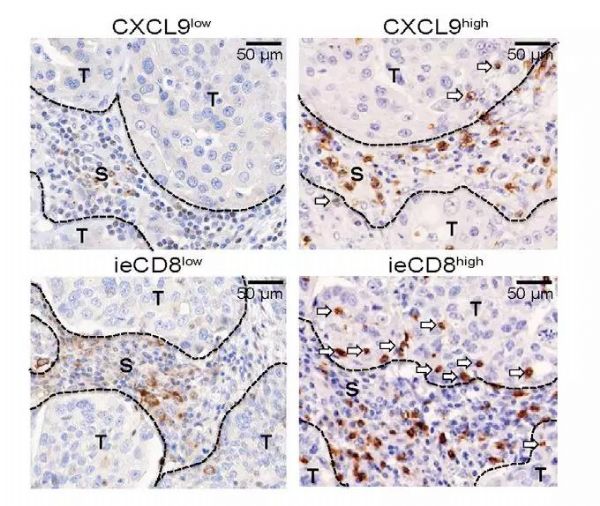
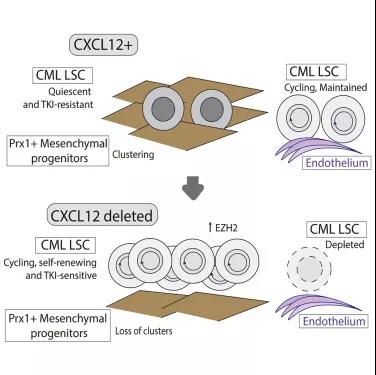
近期的Cancer Cell发表了一篇题为“Cooperation between Constitutive and Inducible Chemokines Enables T Cell Engraftment and Immune Attack in Solid Tumors”的文章。在本文中,研究人员发现趋化因子CCL5和CXCL9与实体瘤中的CD8+ T细胞浸润有关,并且具有CCL5和CX
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Cell#
39
#cancer cell#
31
#CEL#
39
#肿瘤细胞#
39
#趋化因子#
42
666
79
好
79