Circ-Heart Fail:激活的T淋巴细胞是缺血性心力衰竭病理重构的重要机制
2017-03-19 xing.T MedSci原创
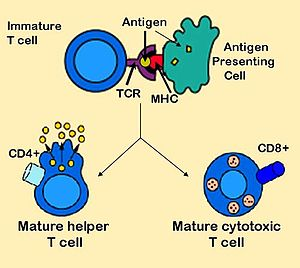
在慢性缺血性心衰中,CD4+T淋巴细胞是整体增加并激活,并且Th2(vs. Th1)和Th17(vs. Treg)在心脏衰竭中占优势,另外,脾脏记忆T细胞也增加。心衰个体的心脏和脾脏T细胞可诱导心脏损伤和重塑,并在过继性转移上保留记忆。
不适当的持续炎症是慢性缺血性心力衰竭(HF)的一个标志,然而,T淋巴细胞在这其中的病理生理作用尚不清楚。近日,心血管领域权威杂志Circ-Heart Fail上针对这一问题发表了一篇研究文章。
研究人员将成年C57BL/6小鼠进行永久冠状动脉结扎。与假手术组相比,HF小鼠(结扎后8周)具有以下特点:(1)显著性(P<0.05)增加循环中CD3+CD8+细胞毒性和CD3+CD4+辅助性T淋巴细胞(Th),同时增加Th1、Th2、Th17和调节性T细胞(Treg)CD4+亚群;(2)衰竭心肌中CD8+和CD4+ T细胞明显增加,同时伴有Th1、Th2、Th17和Treg细胞CD4+亚群的增加,并且Th1/Th2比值显著降低,而Th17/Treg比值增大,上调Th2细胞因子;(3)脾脏、纵隔淋巴结的Th1、Th2、Th17细胞和Tregs明显增加,脾脏抗原经验效应和记忆性CD4+T细胞增加。
HF小鼠(结扎后4周开始)抗体介导的CD4+T细胞耗竭,可以降低CD4+T细胞的心肌浸润,并且阻止进一步的左心室扩大和肥厚,而从供体HF小鼠过继性转移脾脏CD4+T细胞(以及在较小程度上,心脏CD3+T细胞)可以诱导接受小鼠长期的左室功能不全、纤维化和肥厚。
在慢性缺血性心衰中,CD4+T淋巴细胞是整体增加并激活,并且Th2(vs. Th1)和Th17(vs. Treg)在心脏衰竭中占优势,另外,脾脏记忆T细胞也增加。心衰个体的心脏和脾脏T细胞可诱导心脏损伤和重塑,并在过继性转移上保留记忆。
原始出处:
Shyam S. Bansal, et al. Activated T Lymphocytes are Essential Drivers of pathological Remodeling in Ischemic Heart Failure. Circulation:heart failure. 2017. https://doi.org/10.1161/CIRCHEARTFAILURE.116.003688
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#缺血性#
27
#淋巴细胞#
29
#ART#
35
#HEART#
0
#T淋巴细胞#
50
很好的学习资料,谢谢了。
53
非常好的研究
46