Ann Oncol:顺铂+西妥昔单抗+再放疗对于复发性或第二原发性头颈部鳞状细胞癌患者可行
2018-01-19 陶白 肿瘤资讯
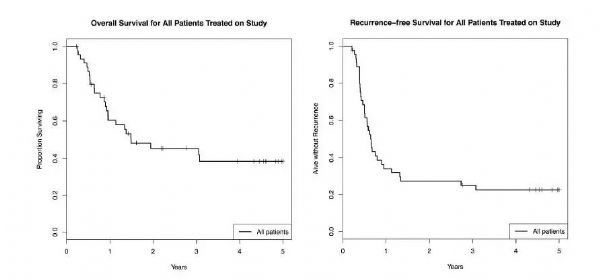
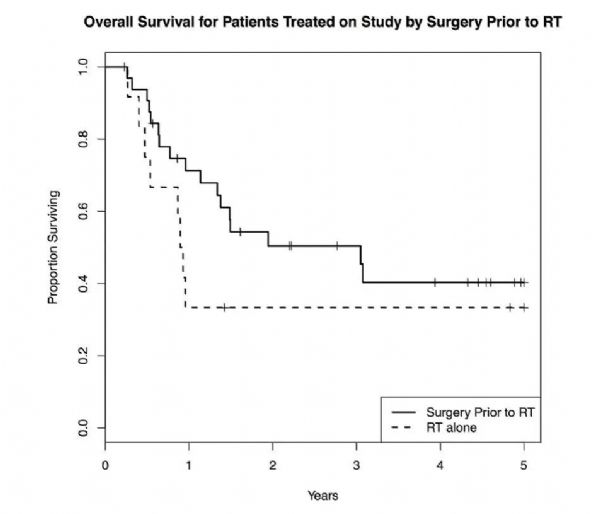
头颈部鳞状细胞癌患者外照射治疗后,常会发生局部区域复发,造成死亡。对于复发性或第二原发性头颈部鳞状细胞癌患者,哪种治疗方案有效性强,且安全性高?美国克里夫兰大学医院凯斯西储大学放射肿瘤系Min Yao博士给出了一个可行的方案。1月15日,《Annals of Oncology》对其研究结果进行了报道。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Oncol#
24
#西妥昔#
26
#铂#
34
#细胞癌#
41
#原发性#
32
#复发性#
32
#头颈部鳞状细胞癌#
27
#头颈部#
28
#颈部#
22
学习了谢谢作者分享!
67