颈后路单节段双开门椎管成形术治疗黄韧带钙化症一例
2019-01-23 乐晓峰 骨科临床与研究杂志
患者女,72岁,因渐进性右侧肢体发凉1年,伴走路不稳于2017年2月被收入北京积水潭医院。现病史:1年前,在无明显诱因出现右侧肢体发凉,涉及范围为前臂至指尖及小腿至足底,伴头痛;后出现走路不稳、四肢无力;4个月前,出现左上肢剧烈疼痛,范围自上臂至前臂外侧,咳嗽时双手指尖有轻微麻木感。既往无特殊病史。入院体格检查:一般情况可,痛苦面容;右侧肢体皮温较对侧低,双侧肱、桡动脉及足背动脉搏动正常;左上肢因
临床资料
患者女,72岁,因渐进性右侧肢体发凉1年,伴走路不稳于2017年2月被收入北京积水潭医院。现病史:1年前,在无明显诱因出现右侧肢体发凉,涉及范围为前臂至指尖及小腿至足底,伴头痛;后出现走路不稳、四肢无力;4个月前,出现左上肢剧烈疼痛,范围自上臂至前臂外侧,咳嗽时双手指尖有轻微麻木感。既往无特殊病史。入院体格检查:一般情况可,痛苦面容;右侧肢体皮温较对侧低,双侧肱、桡动脉及足背动脉搏动正常;左上肢因肩疼痛抬高困难。专科检查:四肢感觉正常;四肢肌力Ⅳ级;Hoffman征(+),病理反射(+),直线连足试验(+);颈椎日本骨科协会(JOA)评分8分,疼痛视觉模拟评分(VAS)8分。实验室检查结果未见显著异常。
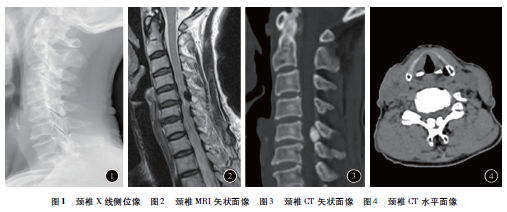
影像学检查:X线未见明显异常(图1);MRI示C5-6后方脊髓受压迫严重(图2);CT示C5-6黄韧带区域左右对称分布2个类圆形高密度影,边缘规则整齐(图3、4)。术前诊断:颈椎黄韧带骨化或钙化导致的合并交感神经症状的脊髓型颈椎病。手术治疗:行全身麻醉,患者取俯卧位,使颈部充分伸展。常规消毒后,取C4-6后正中切口,暴露椎板。用磨钻将C5两侧小关节内侧椎板磨出2个侧沟,再使用磨钻将C5棘突劈开,显露C5-6区域肥厚黄韧带,可见内有白色粉末状组织,去除病灶,送病理学检查,待硬膜渐膨隆、搏动良好后在双侧棘突上钻孔,于C5棘突间用线交叉固定1块梯形人工珊瑚骨,解除脊髓压迫。病理学检查:肉眼可见2个类球形灰白色组织,均约花生米大小,含灰白色粉末状物。镜下检查见纤维软骨及胶原纤维组织伴显著钙化。术后1周,患者右侧肢体皮温恢复正常,可下地循直线行走,头痛及指尖麻木症状消失,左上肢疼痛和抬高程度明显改善,仅余左肩疼痛(术后左肩MRI示肩袖损伤),四肢肌力Ⅳ+级,JOA评分14分,VAS评分2分。术后6个月四肢肌力Ⅴ级,JOA评分15分,VAS评分1分。术后12个月四肢肌力Ⅴ级,JOA评分15分,VAS评分1分。
讨论
患者以右侧肢体发凉起病,双侧肢体血管搏动一致,后出现走路不稳以及肢体疼痛、麻木和肌力下降症状,影像学检查结果示C5-6区域黄韧带病变压迫脊髓,故术前诊断为颈椎黄韧带骨化或钙化导致的合并交感神经症状的脊髓型颈椎病。有文献报道,对症状较轻的黄韧带钙化患者可行口服秋水仙碱治疗或无需干预,故在术前有必要鉴别病灶为骨化还是钙化。黄韧带骨化的基本病理过程为软骨内成骨,其病灶由韧带区、软骨区、软骨钙化区和骨化区4部分组成,软骨钙化区的主要成分为变性的软骨细胞和基质,骨化区多为致密的板层骨;而黄韧带钙化的病理过程则主要是钙盐晶体的沉积,其病灶主要成分为二水焦磷酸钙盐。由此可推测两者的平均CT值也应有明显差异。经测量本例患者病灶CT值为(1100±100)Hu,与文献报道的黄韧带骨化灶平均CT值(547.2±131.4)Hu有较大差异,故术前考虑本例患者黄韧带骨化可能性小。关于颈椎黄韧带骨化和钙化,日本学者报道较多,患者大多数为60岁以上女性。有研究结果表明,黄韧带骨化多见于下胸椎,在颈椎罕见,常累及单节段,从C1-2到C7-T1均可能受累,且受颈椎后凸畸形和后纵韧带骨化等局部因素影响,发生机制与应力相关,其病灶多靠近后纵韧带,与椎板粘连较严重,常呈鸟喙状和土丘状。黄韧带钙化则以颈椎多见,胸椎罕见,常累及1~2个节段,主要受累节段为C4-5和C6-7,其病理机制不明确,常可合并其他关节(如膝、椎间盘、髋、耻骨联合、肩等)的钙盐沉积,其病灶位于黄韧带中央,与椎板粘连较轻,病灶多呈球状,常双侧同时出现。因此,对于本例患者,本文作者术前考虑黄韧带钙化可能性大,术后病理学检查结果证实了这一推测。
患者因疼痛严重,手术意愿强烈,遂放弃保守治疗。对黄韧带源性颈椎病患者,既往多行单纯椎板切除术或单开门椎管成形术,尚未见行双开门椎管成形术治疗的报道。有研究结果表明,椎管成形术的生物力学结果优于椎板切除术。有系统回顾的文献报道,椎管成形术的术后并发症相对更少,减压相对更安全,故在临床应用中更受青睐。关于单开门和双开门椎管成形术的手术指征,通常认为累及3个以下节段的颈椎病变适用单开门术式,累及3个及以上节段的颈椎病则适用双开门术式,但目前仍存在争议。2010年Hirabayashi等比较了椎管成形术中单开门和双开门术式的疗效并总结了这2种术式的手术适应证,认为脊髓型颈椎病合并双侧神经根病变的患者更适用双开门椎管成形术。因黄韧带钙化多造成脊髓双侧受压迫,故本文作者认为本病例更适用双开门椎管成形术。术后本例患者恢复好,交感神经症状消失,患者满意度高。
总之,当患者以肢体发凉和头痛症状起病时,在排除血管病变后,应考虑脊髓型颈椎病的可能性;需采取CT或MRI等敏感性相对更高的影像学检查方法,单纯采用X线检查易导致误诊误治。后路双开门椎管成形术可能更适合治疗黄韧带钙化引起的脊髓型颈椎病。
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#颈后路#
40
#黄韧带#
62
#椎管#
48
#成形术#
37
#钙化症#
35
#韧带#
34