Cancer Cell:科学家找到阻碍免疫系统绞杀癌细胞的“重要障碍”
2017-11-15 佚名 肿瘤免疫细胞治疗资讯
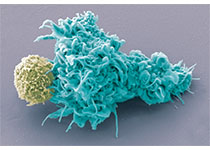
与以前认为的相反,免疫系统的癌症杀伤性T细胞在肿瘤的缺氧环境中更有效,尤其是接近生长因子VEGF-A时。研究人员在卡罗林斯卡研究所发表的一项研究中显示,在转录因子HIF-1a的帮助下,T细胞不仅能够在这种缺氧的微环境中生存下来,而且还能更有效地杀死癌细胞。
与以前认为的相反,免疫系统的癌症杀伤性T细胞在肿瘤的缺氧环境中更有效,尤其是接近生长因子VEGF-A时。研究人员在卡罗林斯卡研究所发表的一项研究中显示,在转录因子HIF-1a的帮助下,T细胞不仅能够在这种缺氧的微环境中生存下来,而且还能更有效地杀死癌细胞。
细胞毒性T细胞对于免疫系统杀死肿瘤细胞的能力是重要的。当T细胞进入肿瘤时,它们被认为是利用转录因子HIF,其与所有转录因子一样是调节基因表达从而调节细胞功能的蛋白质。转录因子HIF也特别能够帮助T细胞适应肿瘤的缺氧微环境。
研究人员现在表明,变体HIF-1a能使T细胞适应这种缺氧的环境,从而成功杀死肿瘤。在分析了变体HIF-2a之后,他们发现T细胞适应缺氧和抗肿瘤的能力不如HIF-1a。
Karolinska医学院细胞与分子生物学系的Randall Johnson教授说:“我们观察到T细胞能够检测氧气,并且通过适应有限的氧气量,他们可以进入缺氧的肿瘤,在其中生存,然后有效地杀死它们。
研究人员还使用小鼠模型试图从其T细胞中敲除VEGF-A(一种使血管生长的生长因子和一种HIF的靶基因)。
约翰逊教授解释说:“这样做,我们发现肿瘤增长,新血管的形成发生了变化。 “这很有趣,因为以前认为当你降低VEGF-A时肿瘤会饿死,我们的研究表明事情比这更复杂,我希望我们的发现能够导致更好的肿瘤治疗,最大限度地发挥T细胞的作用。 ”
原始出处:
Asis Palazon, et al.,An HIF-1α/VEGF-A Axis in Cytotoxic T Cells Regulates Tumor Progression.Cancer Cell.Volume 32, Issue 5, p669–683.e5, 13 November 2017.
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






#Cell#
14
#cancer cell#
27
#CEL#
14
#癌细胞#
18