本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言

53岁男性患者,因发作性胸痛入院,此前于当地就医过程中突发意识丧失。入院后置入冠状动脉支架并药物治疗,患者仍觉胸闷。经检查,发现患者除急性心梗外还伴有急性肝功能损害、急性肾功能不全、血小板减少症等。尽管对症治疗,但入院后20小时内病情急剧恶化,多脏器严重衰竭。患者能否转危为安?对于多器官功能不全综合征应采取哪些治疗措施?详见以下病例?——
我这里说的痛风,指的是急性痛风性关节炎。在高尿酸的基础上,并在一定条件下,尿酸在关节形成结晶,刺激关节滑膜引起非细菌性炎症。一、什么情况下容易痛风发作?绝大多数痛风发生在第一跖趾关节,也就是大脚趾的关节。严重者逐渐向上蔓延,足背、足跟、踝、膝、指、腕和肘等关节。关节着凉(冬天没保暖或夏天吹空调)、饮酒是诱发因素。典型的发作过程是,大量饮酒后,上床睡觉时还没问题,后半夜因脚痛痛醒,而且越来越重,
选择性5-羟色胺再摄取抑制剂(SSRIs)是20世纪80年代陆续开发并试用于临床的一类新型抗抑郁药物。2017年11月,发表在《Stroke》上的一项多中心回顾性分析,对急性缺血性卒中患者住院前使用SSRIs治疗与溶栓后症状性颅内出血(sICH)和功能结局的相关性进行了评估。
男性患者,53岁,因反复心前区闷痛3日、神志不清10分钟入院,自诉有呼吸暂停,经检查诊断为中度阻塞型睡眠呼吸暂停综合征(OSAS)伴急性下壁心肌梗死。作为冠心病的危险因素,OSAS如何影响心血管健康?又有哪些方法治疗OSAS?
急性肺栓塞是一种高发病率和高死亡率的心血管急症,早期诊断和治疗可以明显降低病死率。溶栓治疗是急性肺栓塞重要的治疗措施。溶栓治疗的主要并发症是出血,但溶栓治疗过程中发生猝死少有报道,本文结合2例急性肺栓塞溶栓治疗过程中发生的猝死临床资料,探讨急性肺栓塞溶栓过程中发生猝死的原因,旨在加强对急性肺栓塞溶栓疗法所致严重不良事件的认识。
患者以用力后突发胸痛、心悸为突出表现,急诊处理应以急性胸痛的诊治流程进行。具体步骤是什么?关于宽QRS波心动过速的诊断,有哪些鉴别方法?


梅斯医学MedSci APP
医路相伴,成就大医
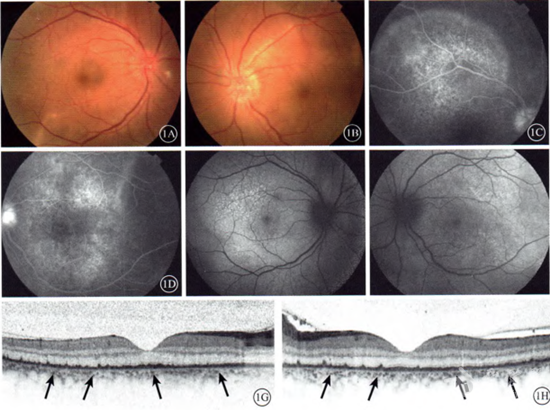
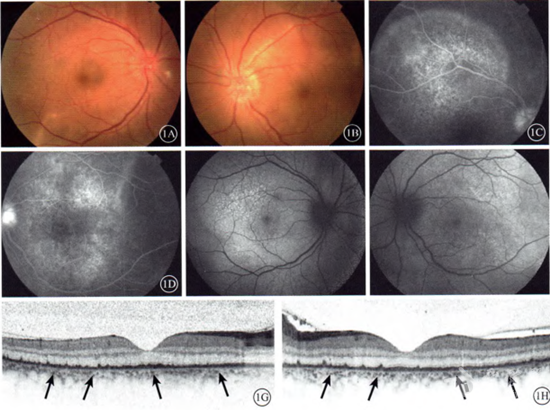
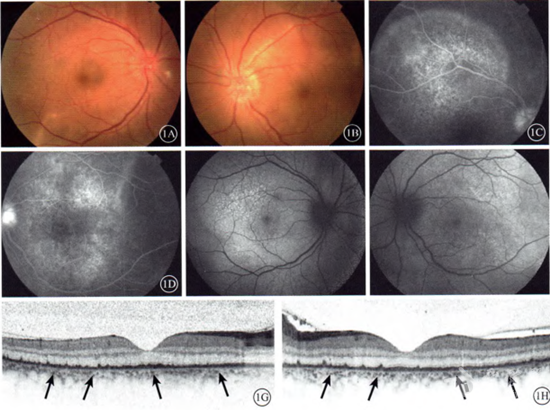
#视网膜炎#
22
#脉络膜#
32
好
65
#视网膜#
35
非常好的文章.学习了
57
非常好的文章.学习了
74