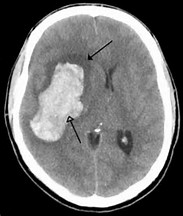
长期玩手机到凌晨 29岁姑娘突患脑梗致右偏瘫
2017-10-15 李佳赟、应红燕 中国新闻网
睡前抱着手机玩游戏、连续两个多月凌晨入睡……近日,长期熬夜的29岁四川姑娘小丽突发脑梗,半边身体动弹不得。在浙江省宁波市李惠利东部医院心内科病房内,小丽躺在床上,看着无力的右侧身体满心悔意。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#脑梗#
28
#偏瘫#
37
学习了
64
好资料学习了!
70
大多数人的生活方式需要改变.
67